Acute incarcerated obturator hernia is a rare cause of thigh pain and is associated with high morbidity and mortality.
A woman in her eighties, who was being evaluated for significant involuntary weight loss, was admitted to the emergency department due to vomiting and the sudden onset of acute pain in her right thigh. The pain was constant and worsened with movement. Clinical examination revealed a highly tender point in the proximal medial region of her right thigh. There was no indication of trauma.
The patient was referred for an X-ray of the right hip to investigate a possible pathological fracture. No fracture or misalignment was observed, and she was admitted to the orthopaedic department for pain management and mobilisation. She was discharged the next day despite persistent pain and vomiting. On day three, the patient was readmitted to the emergency department with the same symptoms. She was afebrile, but due to mildly elevated infection markers, leukocytes at 13.5 × 109/L (reference range 4.1–9.8 × 109/L) and CRP at 60 mg/L (< 5 mg/L), a chest X-ray was performed, revealing basal confluent consolidations in the right lung, raising suspicion of a pneumonic infiltrate. The patient was transferred to the medical ward for observation. Antibiotics were not initated due to minimal respiratory symptoms.
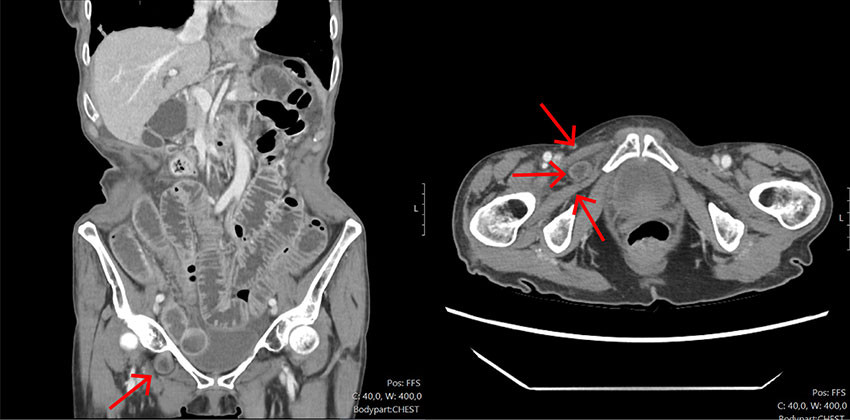
On day four, the woman's condition deteriorated, presenting with tachycardia (heart rate of 119 bpm), a respiratory rate of 28 breaths per minute (normal range: 12–16), and a fever of 38.1°C. Her CRP level also increased from 50 to 250 mg/L. Piperacillin-tazobactam was initiated intravenously at a weight-adjusted dose of 2 g x 4, and she was referred for a CT scan of the chest/abdomen/pelvis due to suspected sepsis from an abdominal focus. The CT scan revealed an incarcerated loop of small bowel protruding through the right obturator canal and pre-obstructive small bowel dilation, consistent with an acute, irreducible obturator hernia (Figures 1a and 1b). The on-call surgeon was promptly consulted, and the patient was scheduled for emergency surgery.
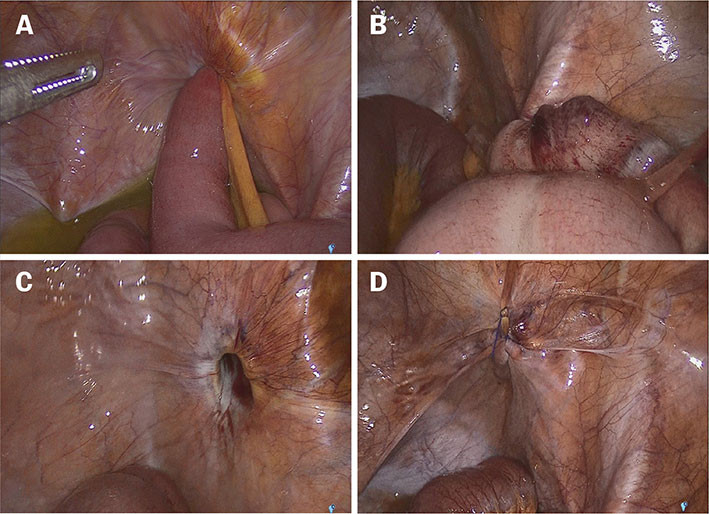
During laparoscopy under general anaesthesia, an incarcerated small bowel loop was found in the obturator canal, consistent with the CT findings (Figure 2a). The bowel was carefully reduced, with no signs of necrosis or perforation. After the hernia was reduced, the patient experienced hypotension, with blood pressure of 98/37 mmHg. Intraoperative arterial blood gas analysis showed pH 7.22 (7.36–7.44), PCO2 (a) 7.0 (4.7–6.0 kPa), PO2 (a) 15.0 (> 8.7 kPa), HCO3 19 (22–26 mmol/L), base excess -6.6 (-1.9–4.5 mmol/L), Cl 104 (98–107 mmol/L), and lactate 1.0 (0.4–1.3 mmol/L), consistent with mixed respiratory and metabolic acidosis. The hypercapnia was presumed to be caused by perioperative absorption of insufflated CO2 gas from the peritoneum into the capillary network. Norepinephrine infusion was initiated at 0.04 mcg/kg/min, and minute ventilation was increased to correct the acidosis. The reduced small bowel segment was re-evaluated and was considered still viable, with no need for resection (Figure 2b). The hernia defect was closed with primary sutures using non-absorbable, knot-free monofilament barbed suture (V-Loc) (Figures 2c and 2d) to minimise surgery time due to the patient's deteriorating condition.
The patient was extubated immediately after surgery and observed in the intensive care unit until the following day. Vasopressors and a decompression nasogastric tube were removed on the first postoperative day. She was then transferred to the surgical ward. Bowel function resumed on the second postoperative day. Antibiotics were discontinued on the third postoperative day. On the same day, she was also transferred back to the medical ward for further evaluation of her weight loss.
Discussion
Obturator hernia is a rare cause of intestinal obstruction and accounts for < 1 % of all abdominal wall hernias (1). The condition was first described by the French surgeon Pierre Roland Arnaud de Ronsil in 1724 and has previously been discussed in this journal (2). It is difficult to diagnose due to unspecific clinical presentation, and for the same reason, it is associated with high morbidity and mortality.
About 90 % of patients with incarcerated obturator hernia experience abdominal pain, nausea and vomiting (3), and half report pain medially and proximally in the thigh during hip internal rotation, known as the Howship-Romberg sign (4). The thigh pain is due to compression of a cutaneous branch of the obturator nerve in the obturator canal. The condition is more common on the right side, as the opening of the left obturator canal is often covered by the sigmoid colon. The patient in this case report had typical symptoms and clinical findings, which could have led to suspicion of the condition upon initial assessment in the emergency department.
Incarcerated obturator hernia is most common in older patients and slim women, and is often referred to as 'little old lady's hernia' due to several structural changes in the pelvis. Anatomically, the female pelvis is wider, the course of the obturator canal is more oblique than in men, and multiparity results in a looser pelvic floor. With age-related loss of muscle mass and fat tissue, or with general weight loss, the 'fat pad' surrounding the artery, vein and obturator nerve passing through the obturator canal disappears. In combination, this leads to the expansion of the obturator canal, making it more susceptible to herniation.
Acute incarcerated obturator hernia requires urgent surgery to relieve the intestinal obstruction and assess whether the hernia content is viable. The choice of surgical technique depends on both the patient's circulatory and respiratory condition and the available expertise. Laparoscopy is suitable because the obturator canal is located deep in the pelvis and because it allows for preperitoneal mesh repair. There is no consensus on whether mesh should be placed during concurrent bowel resection, but the latest guidelines permit this when there is little to no contamination of the abdominal cavity (5). The incidence of recurrent obturator hernia after treatment with primary suturing is 10–20 %, compared to 2–3 % after mesh repair (6, 7). We chose to close the hernia defect with primary suturing due to the patient's altered physiology during the procedure. The patient can be considered for outpatient elective mesh repair at a later date.
We would like to thank the Department of Radiology at Haraldsplass Deaconess Hospital for supplying the CT images.
The patient has consented to publication of the article.
The article has been peer-reviewed.
- 1.
Holm MA, Baker JJ, Andresen K et al. Epidemiology and surgical management of 184 obturator hernias: a nationwide registry-based cohort study. Hernia 2023; 27: 1451–9. [PubMed][CrossRef]
- 2.
Waage S. Inkarserert obturatorhernie. Tidsskr Nor Legeforen 2019; 139. doi: 10.4045/tidsskr.19.0100. [PubMed][CrossRef]
- 3.
Mantoo SK, Mak K, Tan TJ. Obturator hernia: diagnosis and treatment in the modern era. Singapore Med J 2009; 50: 866–70. [PubMed]
- 4.
Kammori M, Mafune K, Hirashima T et al. Forty-three cases of obturator hernia. Am J Surg 2004; 187: 549–52. [PubMed][CrossRef]
- 5.
Stabilini C, van Veenendaal N, Aasvang E et al. Update of the international HerniaSurge guidelines for groin hernia management. BJS Open 2023; 7. doi: 10.1093/bjsopen/zrad080. [PubMed][CrossRef]
- 6.
Burla MM, Gomes CP, Calvi I et al. Management and outcomes of obturator hernias: a systematic review and meta-analysis. Hernia 2023; 27: 795–806. [PubMed][CrossRef]
- 7.
Kawanaka H, Hiroshige S, Kubo N et al. Therapeutic Strategy for Incarcerated Obturator Hernia Using Preoperative Manual Reduction and Laparoscopic Repair. J Am Coll Surg 2018; 226: 891–901. [PubMed][CrossRef]
Ved Sykehuset Østfold har vi siden 2014 brukt CT av bekken med hofter som primærdiagnostikk hos voksne i en årrekke (1). CT har bedre sensitivitet og spesifisitet for skjelettskader i denne regionen, og ville også vist den aktuelle patologien hos denne pasienten. Tid for revisjon av retningslinjene?
Litteratur:
1) Liborg IK, Sorteberg A, Larsen ASF et al. CT som primærdiagnostikk ved mistenkt hoftebrudd. Tidsskr Nor Legeforen 2023; 143.doi: 10.4045/tidsskr.23.0453