Incidence and case fatality of acute myocardial infarction in Norway 2013–2021
Main findings
The incidence of acute myocardial infarction decreased by an average of 3.8 % per year in the period 2013–2021.
The proportion of patients who died within 30 days fell in patients admitted to hospital with myocardial infarction without ST segment elevation (NSTEMI), but not in patients admitted with myocardial infarction with ST segment elevation (STEMI).
In 2021, about 1 in 5 patients with acute myocardial infarction died within 30 days.
Over the past 100 years, ischemic heart disease mortality has changed considerably in Norway. In the first half of the last century, mortality steadily increased, except for a marked decrease during World War II (1). Mortality then rose substantially in the post-war years, peaking in the 1970s, and then falling again just as dramatically (2).
The mortality of a disease depends on how many people are affected (incidence) and the proportion of those who die (case fatality). In the 1960s, the Norwegian epidemiologist Knut Westlund documented in several classic studies that the post-war increase in the mortality of acute myocardial infarction was correlated with increased incidence (3). The decline in mortality from myocardial infarction in Norway after 1970 is associated with changes in both incidence (4) and case fatality (5). These analyses are based on data from the Norwegian Patient Registry (6) and do not distinguish between myocardial infarction with ST segment elevation (STEMI) and without ST segment elevation (NSTEMI). This is an important distinction, as STEMI is usually associated with a total occlusion of a coronary artery, leading to greater myocardial injury. This type of infarction is associated with higher case fatality than NSTEMI and requires different treatment in the acute phase (7).
Since 2012, Norwegian hospitals have been required to register patients who are admitted with myocardial infarction in the Norwegian Myocardial Infarction Registry (8, 9). The registry contains information about risk factors, patient characteristics and the type of myocardial infarction. In this study, we linked data from the Norwegian Myocardial Infarction Registry, the Norwegian Patient Registry and the Norwegian Cause of Death Registry to obtain a more comprehensive picture of all types of myocardial infarction than in previous studies. The aim was to examine incidence, case fatality and patient characteristics for different types of myocardial infarction in the period 2013–2021.
Material and method
Data collection
The Norwegian Myocardial Infarction Registry (9), the Norwegian Patient Registry (6) and the Norwegian Cause of Death Registry (10) were used to identify all patients registered with acute myocardial infarction (ICD-10 codes I21 and I22) in national health registries in the period 1 January 2013 to 31 December 2021 (11). We included patients with a Norwegian personal identification number who were over the age of 20 years when the myocardial infarction occurred. The three registries were linked using serial numbers/encrypted personal identification numbers.
The Norwegian Myocardial Infarction Registry is a national medical quality registry that contains information on patients treated in Norwegian hospitals for acute myocardial infarction (9). The registry is not consent-based. The coverage rate is approximately 90 % compared to the Norwegian Patient Registry (9).
The Norwegian Myocardial Infarction Registry contains 80 variables, including age and sex, type of myocardial infarction (STEMI, NSTEMI, unknown), smoking habits (never, current smoker, ex-smoker, unknown), the first LDL cholesterol level (mmol/L) measured after admission, ongoing medication for hypertension (yes, no, unknown), diabetes mellitus (yes, no, unknown), as well as the highest values of troponin-T and troponin-I (ng/L) measured during hospitalisation.
The Norwegian Patient Registry contains personally identifiable information about discharge diagnoses for patients in Norwegian hospitals from 2008 (6). The Norwegian Cause of Death Registry includes underlying and contributory causes of death (10). In this study, the category 'Out-of-hospital deaths from myocardial infarction' includes patients registered in the Norwegian Cause of Death Registry with myocardial infarction as an underlying or contributory cause of death who were not recorded in the Norwegian Myocardial Infarction Registry or the Norwegian Patient Registry as having been admitted to hospital with a myocardial infarction diagnosis.
A first-time infarction event (incident) was defined as the first hospital admission recorded in the Norwegian Myocardial Infarction Registry or the Norwegian Patient Registry with myocardial infarction as the discharge diagnosis, or death with myocardial infarction as an underlying or contributory cause of death without having been registered in the Norwegian Patient Registry or the Norwegian Myocardial Infarction Registry in the preceding five years (12). In this study, a first-time infarction event is defined as an event occurring in a person who has not experienced a myocardial infarction in the five years prior, hence the five-year look-back period. This look-back period was chosen since the Norwegian Patient Registry contains personal identification numbers from 2008.
Thirty-day case fatality is defined as the percentage of first-time infarction events with a fatal outcome within 30 days of the admission date.
The study was approved by the Regional Committee for Medical and Health Research Ethics in South-Eastern Norway. The Norwegian Institute of Public Health assessed the implications for privacy and granted permission to link data.
Statistical analyses
We calculated annual incidence rates in ten-year age intervals using the population of Norway at the start of each calendar year as the denominator. Age-adjusted incidence rates per 100 000 inhabitants were calculated using the direct method, with ten-year age strata and the Norwegian population in 2017 as the standard population. Age adjustment of case fatality was performed using the direct method with ten-year age strata and the population in the Norwegian Myocardial Infarction Registry in 2017 as the standard population.
Time trends were examined using Poisson regression, with the year of the infarction event and age as continuous, independent variables. The incidence rate ratio (IRR) from Poisson regression, along with the corresponding 95 % confidence interval (CI), expresses the mean annual percentage change from the previous year, adjusted for age. The Wald test was used to analyse gender differences in the incidence trend. Logistic regression with the covariates of sex, age, hypertension, diabetes and smoking was used to examine gender differences in case fatality.
Results
Incidence
The number of patients with a first-time infarction event decreased from 14 361 (391/100 000) in 2013 to 11 264 (271/100 000) in 2021, corresponding to a mean reduction in age-adjusted incidence rates of 3.8 % per year (95 % CI 3.6 to 4.1; p < 0.001) (Table 1) (see Table 1 in the appendix on tidsskriftet.no). The incidence of STEMI decreased by 2.3 % per year (p < 0.001), NSTEMI incidence decreased by 3.1 % per year (p < 0.001), and the incidence of out-of-hospital deaths decreased by 6.5 % per year (p < 0.001). There was a significant decline in the incidence of all types of myocardial infarction, as well as STEMI and NSTEMI, among both men and women in all age groups over 20 years (Figure 1, Table 2).
Table 1
Number of first-time myocardial infarction events and incidence per 100 000 inhabitants in Norway in 2013, 2017 and 2021 based on registry linkage. CI = confidence interval.
| 2013 | 2017 | 2021 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type of myocardial infarction | No. | Age-adjusted incidence per 100 000 | No. | Age-adjusted incidence per 100 000 | No. | Age-adjusted incidence per 100 000 | Mean % change in age-adjusted incidence per year (95 % CI) | |||
| All myocardial infarctions¹ | 14 361 | 391 | 13 110 | 332 | 11 264 | 271 | -3.8 (-3.6 to -4.1) | |||
| Admitted to hospital² | 12 388 | 338 | 11 463 | 290 | 10 041 | 243 | -3.5 (-3.2 to -3.7) | |||
| STEMI³ | 3 941 | 81 | 2 878 | 72 | 2 719 | 63 | -2.3 (-1.8 to -2.8) | |||
| NSTEMI⁴ | 7 160 | 195 | 7 198 | 181 | 6 388 | 148 | -3.1 (-2.8 to -3.4) | |||
| Out-of-hospital deaths from myocardial infarction⁵ | 1 973 | 54 | 1 647 | 42 | 1 223 | 29 | -6.5 (-5.9 to -7.1) | |||
¹ Registered in the Norwegian Myocardial Infarction Registry or Norwegian Patient Registry or Norwegian Cause of Death Registry.
² Registered in the Norwegian Myocardial Infarction Registry or Norwegian Patient Registry. The number is higher than the sum of STEMI and NSTEMI events because it also includes patients registered in the Norwegian Myocardial Infarction Registry with unknown type of myocardial infarction and patients not registered in the Norwegian Myocardial Infarction Registry, but in the Norwegian Patient Registry.
³ Registered in the Norwegian Myocardial Infarction Registry as myocardial infarction with ST elevation.
⁴ Registered in the Norwegian Myocardial Infarction Registry as myocardial infarction without ST elevation.
⁵ Registered in the Norwegian Cause of Death Registry but not in the Norwegian Myocardial Infarction Registry or the Norwegian Patient Registry.
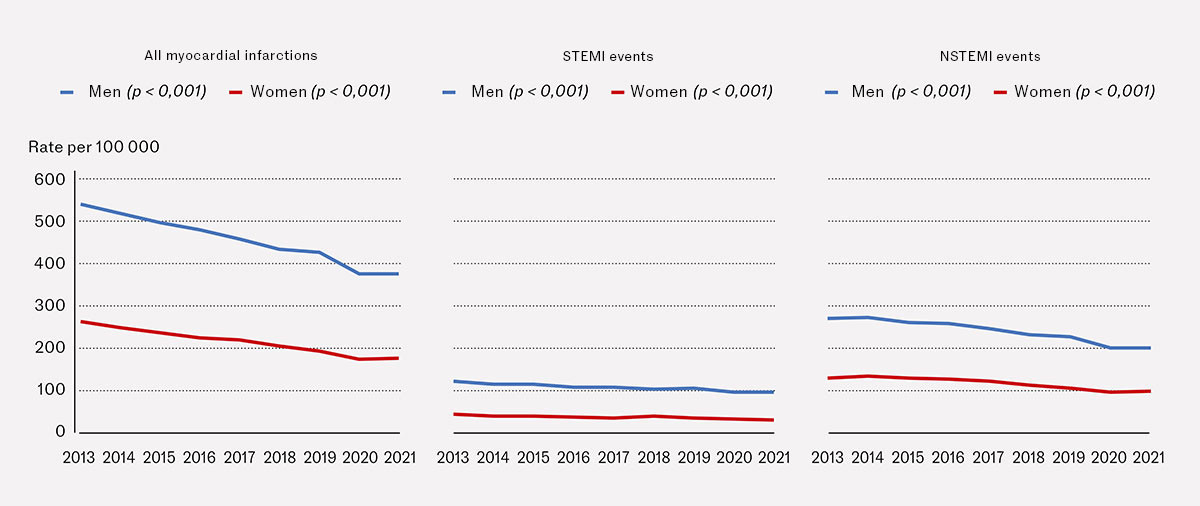
Table 2
Mean annual change in the incidence of acute myocardial infarction by sex and age in Norway 2013–21 based on registry linkage. STEMI = myocardial infarction with ST segment elevation, NSTEMI = myocardial infarction without ST segment elevation.
| Annual change in incidence¹ (%) | ||
|---|---|---|
| Age | Men | Women |
| All myocardial infarctions² | ||
| 20–49 years | -5.3 (-4.4 to -6.3) | -6.1 (-4.3 to -8.0) |
| 50–79 years | -3.1 (-2.8 to -3.5) | -3.3 (-2.8 to -3.8) |
| > 80 years | -6.1 (-5.5 to -6.6) | -6.3 (-5.8 to -6.8) |
| > 20 years, age-adjusted | -3.2 (-2.9 to -3.5) | -5.0 (-4.6 to -5.3)³ |
| STEMI events⁴ | ||
| 20–49 years | -6.1 (-4.6 to -7.6) | -5.8 (-2.2 to -9.2) |
| 50–79 years | -2.2 (-1.6 to -2.9) | -3.2 (-2.1 to -4.3) |
| ≥ 80 years | -2.7 (-1.1 to -4.2) | -2.9 (-1.4 to -4.3) |
| ≥ 20 years, age-adjusted | -2.0 (-1.4 to -2.5) | -3.1 (-2.3 to -4.0)⁵ |
| NSTEMI events⁴ | ||
| 20–49 years | -4.6 (-3.2 to -5.9) | -5.2 (-2.7 to -7.7) |
| 50–79 years | -2.9 (-2.4 to -3.3) | -2.9 (-2.2 to -3.6) |
| > 80 years | -5.1 (-4.4 to -5.8) | -4.8 (-4.1 to -5.5) |
| > 20 years, age-adjusted | -2.7 (-2.3 to -3.0) | -3.9 (-3.4 to -4.4)³ |
¹ Age-specific mean annual change (%) in incidence, calculated using Poisson regression. Values for 20 years and older are age-adjusted.
² Registered in the Norwegian Myocardial Infarction Registry or Norwegian Patient Registry or Norwegian Cause of Death Registry.
³ Significant difference from men (p < 0.001).
⁴ Registered in the Norwegian Myocardial Infarction Registry.
⁵ Significant difference from men (p = 0.027).
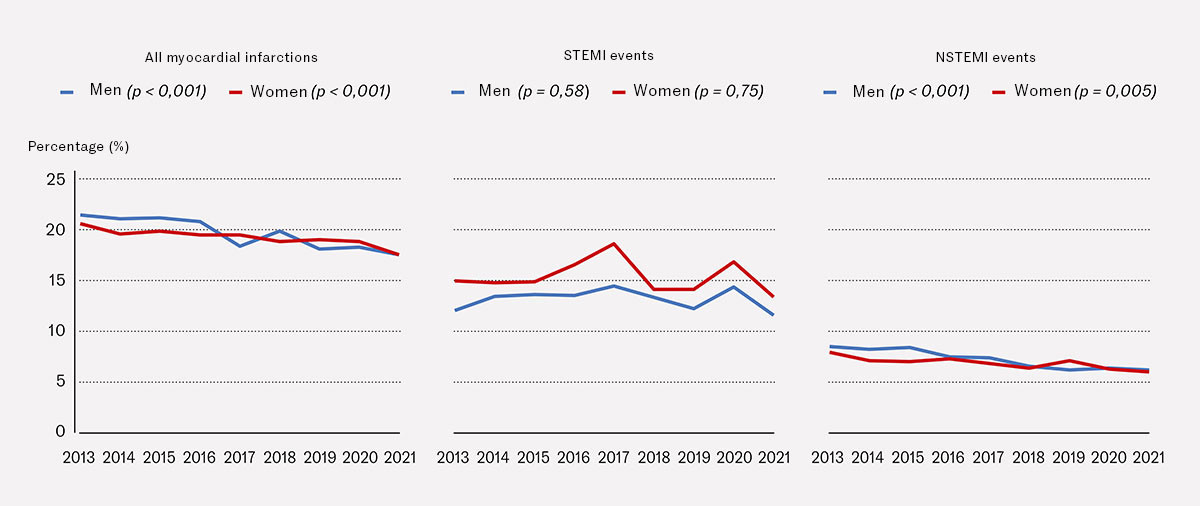
30-day case fatality
30-day age-adjusted case fatality for all myocardial infarctions decreased from 21.2 % in 2013 to 17.5 % in 2021 (p < 0.001). Case fatality after NSTEMI fell from 8.2 % to 6.0 % (p < 0.001), while case fatality after STEMI remained unchanged. The trends were similar for men and women. The case fatality after STEMI events was approximately twice as high as after NSTEMI events (Figure 2, see Table 1 in the appendix).
Patient characteristics
STEMI patients were younger than NSTEMI patients. In the STEMI group, there were more men and smokers, fewer with hypertension and diabetes, and troponin levels were approximately ten times higher (Table 3, see Table 2 in the appendix). There were no significant changes over time in age, gender distribution or LDL cholesterol, but the proportion of smokers fell while the proportion with diabetes increased. The highest troponin-T and troponin-I levels remained unchanged over time for STEMI patients. For NSTEMI patients, a significant decline was observed over time in the highest troponin-I level (Table 3), and the highest troponin-T level was also lower in 2019 (p = 0.011) and 2020 (p = 0.009) than in 2013 (see Table 2 in the appendix).
Table 3
Characteristics of patients admitted to hospital with a first-time STEMI or NSTEMI in 2013, 2017 and 2021, who were registered in the Norwegian Myocardial Infarction Registry
| STEMI | NSTEMI | |||||
|---|---|---|---|---|---|---|
| 2013 | 2017 | 2021 | 2013 | 2017 | 2021 | |
| Number | 3 941 | 2 878 | 2 719 | 7 160 | 7 198 | 6 388 |
| Age, year, mean (SD) | 66 (13) | 66 (13) | 67 (13)¹ | 72 (14) | 72 (13) | 72 (13) |
| Men, % | 71 | 73 | 73¹ | 62 | 62 | 64 |
| Smokers, % | 40 | 35 | 34¹ | 26 | 23 | 22¹ |
| LDL cholesterol, mmol/L², mean (SD) | 3.4 (1.1) | 3.4 (1.1) | 3.3 (1.1) | 3.1 (1.4) | 3.1 (1.2) | 3.0 (1.2) |
| Hypertension, % | 39 | 37 | 42³ | 51 | 50 | 50 |
| Diabetes mellitus, | 13 | 16 | 17¹ | 20 | 21 | 22¹ |
| Troponin-T, ng/L⁴, median (upper and lower quartile) | 3 288 | 3 167 | 3 359 | 317 | 298 | 306 |
| Troponin-I, ng/L⁴, median (upper and lower quartile) | 13 229 | 15 553 | 14 683 | 1 373 | 985 | 1 021 |
¹ P < 0.001 for change from 2013 to 2021.
² First measurement during hospitalisation.
³ p = 0.009 for change from 2013 to 2021.
⁴ Highest level measured during hospitalisation.
Gender differences
The age-adjusted incidence of all types of myocardial infarction was twice as high for men as for women (Figure 1). The decrease in incidence was less pronounced for men than for women (Table 2).
Throughout the study period, STEMI case fatality was higher for women than men and NSTEMI case fatality was lower (Figure 2). For the period as a whole, STEMI case fatality was 21 % higher for women than men (age-adjusted OR, 1.21; 95 % CI 1.10 to 1.32; p < 0.001). The difference was significant after adjusting for hypertension, diabetes and smoking in addition to age (multivariable adjusted OR, 1.13; 95 % CI 1.02 to 1.25; p = 0.016). NSTEMI case fatality was 9 % lower for women than men for the period as a whole (age-adjusted OR, 0.91; 95 % CI 0.84 to 0.98; p = 0.015). The difference was significant after adjusting for hypertension, diabetes and smoking in addition to age (multivariable adjusted OR, 0.88; 95 % CI 0.81 to 0.95; p < 0.001). Table 3 in the appendix shows gender-specific numbers of myocardial infarctions and the number of deaths per year.
Discussion
In this study, we observed a significant decline in the incidence of acute myocardial infarction during the period 2013–21. Despite the decrease in case fatality, acute myocardial infarction remains a serious condition. In 2021, nearly one in five patients died within 30 days. Many deaths occur in out-of-hospital settings. The falling incidence is due to fewer patients being treated in hospitals for STEMI and NSTEMI and a reduction in out-of-hospital deaths.
Previous studies from Norway (4, 13) and other countries (14) have reported a decreasing incidence of myocardial infarction. In some countries, this decline began as early as the 1980s (14). Our data suggest that the decline continued into the 2000s and applied to both sexes and all age groups. Data from the Swedish National Board of Health and Welfare for the period 2013–21 (15) show remarkable similarities between Swedish and Norwegian trends. In Sweden, the incidence fell by 3.2 % per year to 298/100 000 in 2021, while in Norway, the decrease was 3.8 % per year to 271/100 000 in the same year.
National data on the incidence and case fatality of STEMI and NSTEMI events have not been published previously. Our findings align with results from a study in Tromsø, which found that the incidence of myocardial infarction decreased by 3.0 % per year in the period 1995–2010 (13). In both studies, a marked decline was observed in the incidence of STEMI events and out-of-hospital deaths. This supports the hypothesis that a key driver for the reduced mortality from myocardial infarction in Norway is the reduction in the number of people who experience myocardial infarction, as opposed to a reduction in case fatality among patients admitted to hospital. Studies in other countries have reported similar findings. In the international MONICA study conducted in the 1980s and 1990s, it was found that approximately three-quarters of the decrease in mortality from myocardial infarction could be attributed to reduced incidence and one-quarter to reduced case fatality (14).
More favourable levels of the three classic risk factors – cholesterol, smoking and blood pressure – are likely the main reason for the drop in the number of myocardial infarctions. Studies have shown that these three risk factors account for most of the changes in incidence within a population (16, 17). In the Tromsø Study, it was found that 66 % (95 % CI 48 to 97) of the decline in ischemic heart disease incidence from 1995 to 2010 could be attributed to changes in modifiable risk factors such as cholesterol, blood pressure, smoking and inactivity (13).
Surveys of cardiovascular health in three Norwegian counties showed that the decline in cholesterol, blood pressure and smoking began in the early 1970s (18). More recent data suggests that this favourable trend continues (19). The reduction in cholesterol is primarily attributed to dietary changes (20, 21). Even after statins were introduced in the 1990s, these account for less than 30 % of the cholesterol reduction in the population (22). Lower risk factor levels may also have contributed to the decline in case fatality (23).
National data from Sweden shows that 28-day case fatality after all myocardial infarctions was 22 % in 2021 (15), while the 30-day case fatality in Norway was 17.5 % in 2021. A Danish study covering the period 2004–08 shows a slightly higher 30-day case fatality in hospital settings (14.8 %) (24) than what we found for 2012 (10.1 %). This suggests that case fatality after myocardial infarction may be somewhat lower in Norway than in other Scandinavian countries.
It is striking that during the period 2013–2021 there was no change in case fatality for STEMI, in contrast to NSTEMI. Previous studies from the United States (25) and Norway (13) also found no change in STEMI case fatality between 1995 and 2008, despite the introduction of new treatment methods during this period, such as percutaneous coronary intervention. In both studies, and in our study, markers of myocardial injury decreased in NSTEMI cases, but not in STEMI cases. This may indicate that an increasing proportion of NSTEMI patients had less extensive myocardial injuries, potentially leading to lower case fatality.
It is well-known that men have approximately twice the risk of myocardial infarction than women, and this increased risk is lifelong (26). However, studies on gender differences in case fatality have yielded inconsistent findings (27, 28). We found that case fatality was higher in women than men in STEMI cases. This has also been observed in other studies and may be due to longer delays between symptom onset and hospital admission (27) and/or fewer women receiving reperfusion therapy within the recommended timeframe (29).
A strength of our study is that we used information from all three national registries containing data on myocardial infarction. Using data from both the Norwegian Myocardial Infarction Registry and the Norwegian Patient Registry was found to have a positive predictive value of 97 % and a sensitivity of 92 %, measured against a reference standard (30).
The study also has several weaknesses. Concerns have been raised about the quality of data in the Norwegian Cause of Death Registry, particularly for ischemic heart disease (10, 31). The proportion of misdiagnoses is likely higher for out-of-hospital deaths than for patients admitted to hospital. However, we are not aware of any changes in coding practices during the study period that could have affected our incidence calculations. Coding errors have been identified in the Norwegian Patient Registry (32). A validation study nevertheless showed a high positive predictive value and completeness (sensitivity) for acute myocardial infarction (30). The five-year look-back period means that a number of myocardial infarction cases in our study (perhaps 5–7 %) are not first-time infarctions, but recurrent events (12). This will slightly reduce the observed decrease in incidence (12), but does not weaken our findings.
Conclusion
We found a declining incidence of acute myocardial infarction from 2013 to 2021 across younger, middle-aged and older men and women. Case fatality decreased for all types of myocardial infarction combined, driven by a lower incidence of both STEMI and NSTEMI events and out-of-hospital deaths, as well as lower case fatality following NSTEMI events. Case fatality after STEMI remained unchanged.
The article has been peer-reviewed.
- 1.
Strøm A, Jensen RA. Mortality from circulatory diseases in Norway 1940-1945. Lancet 1951; 1: 126–9. [PubMed][CrossRef]
- 2.
Vollset SE, Tell GS, Thelle DS et al. Dødelighet og dødsårsaker i Norge gjennom 60 år – 1951 – 2010. Folkehelseinstituttet. https://www.fhi.no/publ/2012/dodelighet-og-dodsarsaker-i-norge-g/ Accessed 10.9.2024.
- 3.
Westlund K. Further observations on the incidence of myocardial infarction in Oslo. J Oslo City Hosp 1965; 15: 201–31. [PubMed]
- 4.
Sulo G, Igland J, Vollset SE et al. Trends in incident acute myocardial infarction in Norway: An updated analysis to 2014 using national data from the CVDNOR project. Eur J Prev Cardiol 2018; 25: 1031–9. [PubMed][CrossRef]
- 5.
Sulo G, Igland J, Sulo E et al. Mortality following first-time hospitalization with acute myocardial infarction in Norway, 2001-2014: Time trends, underlying causes and place of death. Int J Cardiol 2019; 294: 6–12. [PubMed][CrossRef]
- 6.
Bakken IJ, Surén P, Håberg SE et al. Norsk pasientregister–en viktig kilde for forskning. Tidsskr Nor Legeforen 2014; 134: 12–3. [PubMed][CrossRef]
- 7.
ESC Scientific Document Group. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J 2023; 44: 3720–826. [PubMed][CrossRef]
- 8.
Helse- og omsorgsdepartementet. Forskrift om innsamling og behandling av helseopplysninger i Nasjonalt register over hjerte- og karlidelser (Hjerte- og karregisterforskriften). https://lovdata.no/dokument/SF/forskrift/2011-12-16-1250 Accessed 13.7.2024.
- 9.
St. Olavs hospital. Norsk hjerteinfarktregister. https://hjerteinfarktregisteret.no Accessed 15.7.2024.
- 10.
Pedersen AG, Ellingsen CL. Datakvalitet i Dødsårsaksregisteret. Tidsskr Nor Legeforen 2015; 135: 768–70. [PubMed][CrossRef]
- 11.
Helsedirektoratet. ICD-10 Den internasjonale statistiske klassifikasjon av sykdommer og beslektede helseproblemer. 10 revisjon. Oslo: Helsedirektoratet, 2011.
- 12.
Sulo G, Igland J, Vollset SE et al. Effect of the lookback period's length used to identify incident acute myocardial infarction on the observed trends on incidence rates and survival: Cardiovascular Disease in Norway Project. Circ Cardiovasc Qual Outcomes 2015; 8: 376–82. [PubMed][CrossRef]
- 13.
Mannsverk J, Wilsgaard T, Mathiesen EB et al. Trends in modifiable risk factors are associated with declining incidence of hospitalized and nonhospitalized acute coronary heart disease in a population. Circulation 2016; 133: 74–81. [PubMed][CrossRef]
- 14.
Tunstall-Pedoe H, Kuulasmaa K, Mähönen M et al. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet 1999; 353: 1547–57. [PubMed][CrossRef]
- 15.
Socialstyrelsen. 2023-11-29. Statistik om hjärtinfarkter 2022. Sveriges officiella statistik. Hälsa- ochsjukvård, publiseringsår 2023. https://www.socialstyrelsen.se/statistik-och-data/statistik/alla-statistikamnen/hjartinfarkter Accessed 15.7.2024.
- 16.
Magnus P, Beaglehole R. The real contribution of the major risk factors to the coronary epidemics: time to end the "only-50%" myth. Arch Intern Med 2001; 161: 2657–60. [PubMed][CrossRef]
- 17.
Stamler J. Low risk–and the "No more than 50%" myth/dogma. Arch Intern Med 2007; 167: 537–9. [PubMed][CrossRef]
- 18.
Jenum AK, Graff-Iversen S, Selmer R et al. Risikofaktorer for hjerte- og karsykdom og diabetes gjennom 30 år. Tidsskr Nor Laegeforen 2007; 127: 2532–6. [PubMed]
- 19.
Nilsen A, Hanssen TA, Lappegård KT et al. Secular and longitudinal trends in cardiovascular risk in a general population using a national risk model: The Tromsø Study. Eur J Prev Cardiol 2019; 26: 1852–61. [PubMed][CrossRef]
- 20.
Pedersen JI, Tverdal A, Kirkhus B. Kostendringer og dødelighetsutvikling av hjerte- og karsykdommer i Norge. Tidsskr Nor Laegeforen 2004; 124: 1532–6. [PubMed]
- 21.
Johansson L, Drevon CA, Aa Bjørneboe GE. The Norwegian diet during the last hundred years in relation to coronary heart disease. Eur J Clin Nutr 1996; 50: 277–83. [PubMed]
- 22.
Hopstock LA, Bønaa KH, Eggen AE et al. Longitudinal and secular trends in total cholesterol levels and impact of lipid-lowering drug use among Norwegian women and men born in 1905-1977 in the population-based Tromsø Study 1979-2016. BMJ Open 2017; 7. doi: 10.1136/bmjopen-2016-015001. [PubMed][CrossRef]
- 23.
Njølstad I, Arnesen E. Preinfarction blood pressure and smoking are determinants for a fatal outcome of myocardial infarction: a prospective analysis from the Finnmark Study. Arch Intern Med 1998; 158: 1326–32. [PubMed][CrossRef]
- 24.
Schmidt M, Jacobsen JB, Lash TL et al. 25 year trends in first time hospitalisation for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort study. BMJ 2012; 344 (jan25 2). doi: 10.1136/bmj.e356. [PubMed][CrossRef]
- 25.
Yeh RW, Sidney S, Chandra M et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 2010; 362: 2155–65. [PubMed][CrossRef]
- 26.
Albrektsen G, Heuch I, Løchen M-L et al. Lifelong gender gap in risk of incident myocardial infarction. The Tromsø Study. JAMA Intern Med 2016; 176: 1673–9. [PubMed][CrossRef]
- 27.
Bugiardini R, Ricci B, Cenko E et al. Delayed care and mortality among women and men with myocardial infarction. J Am Heart Assoc 2017; 6. doi: 10.1161/JAHA.117.005968. [PubMed][CrossRef]
- 28.
Israeli Thrombolytic Survey Group. Sex differences in management and outcome after acute myocardial infarction in the 1990s: A prospective observational community-based study. Circulation 2000; 102: 2484–90. [PubMed][CrossRef]
- 29.
Gupta A, Barrabes JA, Strait K et al. Sex differences in timeliness of reperfusion in young patients with ST-segment-elevation myocardial infarction by initial electrocardiographic characteristics. J Am Heart Assoc 2018; 7. doi: 10.1161/JAHA.117.007021. [PubMed][CrossRef]
- 30.
Varmdal T, Mathiesen EB, Wilsgaard T et al. Validating acute myocardial infarction diagnoses in national health registers for use as endpoint in research: the Tromsø Study. Clin Epidemiol 2021; 13: 675–82. [PubMed][CrossRef]
- 31.
Alfsen GC, Mæhlen J. Obduksjonens betydning for registrering av dødsårsak. Tidsskr Nor Legeforen 2012; 132: 147–51. [PubMed][CrossRef]
- 32.
Hellevik SB. Feil diagnosekoder gir dårligere styring av helseforetakene. Tidsskr Nor Legeforen 2017; 137: 862–3. [PubMed][CrossRef]
Dette er en veldig viktig og god artikkel, og forfatterne gratuleres! Men det er vanskelig å forstå figur 2 dersom det skal være samme skala på Y-aksen. Letaliteten for alle typer infarkt må vel ligge et sted mellom letaliteten for STEMI og NSTEMI, mens det nå synes som letaliteten for alle typer samlet er høyere enn ved STEMI? Er det korrekt benevning på de tre kurvene?
Tor Ole Klemsdal spør i en kommentar (1) om det er en feil i figur 2 i vår artikkel om insidens og letalitet av akutt hjerteinfarkt i Norge 2013-21 (2), siden letalitet for alle hjerteinfarkt er høyere enn for STEMI. Nei - figuren er korrekt. I teksten under figuren skriver vi: "Letaliteten av alle hjerteinfarkt er høyere enn STEMI- og NSTEMI-letaliteten fordi alle hjerteinfarkt inkluderer fatale hjerteinfarkt utenfor sykehus som var registrert i Dødsårsaksregisteret, men ikke i Norsk hjerteinfarktregister." Norsk hjerteinfarktregister inkluderer kun innlagte pasienter. I figur 2 inkluderer STEMI-infarkt pasienter innlagt i sykehus med STEMI, mens NSTEMI-infarkt inkluderer pasienter innlagt i sykehus med NSTEMI. Alle hjerteinfarkt inkluderer i tillegg også ikke-innlagte pasienter som døde av hjerteinfarkt utenfor sykehus og som er registrert i Dødsårsaksregisteret. Det er en styrke ved norske helseregister at vi ved å koble dem kan få et komplett bilde av forekomst av hjerteinfarkt. Mange studier inkluderer kun pasienter innlagt i sykehus, og utelater den viktige gruppen av pasienter som dør før innleggelse. Når man også inkluderer pasienter som dør utenfor sykehus, finner man betydelig høyere letalitet av hjerteinfarkt enn om man kun inkluderer de som overlever frem til sykehus. De fleste dødsfall av hjerteinfarkt inntreffer utenfor sykehus. Dette er vist i flere studier (3, 4). Hjerteinfarkt er en alvorligere sykdom enn hva man får inntrykk av ved kun å studere de som er innlagt i sykehus.
Litteratur
1. Klemsdal TO. Flott og viktig artikkel. Feil ved figur 2? Tidsskr Nor Legeforen 14.10.2024. https://tidsskriftet.no/2024/10/kommentar/flott-og-viktig-artikkel-feil-ved-figur-2#comment-3291 Lest 14.10.2024.
2. Bønaa KH, Halle KK, Govatsmark RES et al. Insidens og letalitet av akutt hjerteinfarkt i Norge 2013–21. Tidsskr Nor Legeforen 2024; 144. doi: 10.4045/tidsskr.24.0237
3. Salomaa V, Ketonen M, Koukkunen H et al. Decline in out-of hospital coronary heart disease deaths has contributed the main part to the overall decline in coronary heart disease mortality rates among persons 35 to 64 years of age in Finland. The FINAMI study. Circulation 2003; 108: 691-696
4. Dudas, K, Lappas G, Stewart S, Rosengren A. Trends in out-of -hospital deaths due to coronary heart disease in Sweden (1991 to 2006). Circulation 2011; 123: 46-52
Norsk forekomst og dødelighet ved hjerteinfarkt falt i perioden 2013-2021 (1). Bra! Men står det da bra til med hjertehelsen spesielt og allmennhelsen generelt? Nei. I 2023 var overdødeligheten for hjerte-karsykdommer 22,4 %, alle aldersgrupper (2010-2019 referanseår) (2). Overdødeligheten var omtrent 100 % for hypertensjon og 41 % for annen iskemisk hjertesykdom (2). Dødsfall ved hjerteinfarkt var også signifikant høyere enn forventet i 2023 (2).
Blant barn og unge (1-39 år) var overdødeligheten 36,4 % for hjerte-karsykdommer i 2023 (2). Riktignok ikke signifikant på grunn av få observasjoner, men en signifikant overdødelighet på 59,6 % for alle sykdommer i denne aldersgruppen burde alarmere. Sammenlignet med 2013-2019 peker også pilene opp for bruk av hjertemedisin (C – hjerte og kretsløp) blant unge fra og med 2021, og økningen var omtrent 20 % i 2023 (tallene varierer noe etter aldersgrupper som inkluderes) (3).
Så står det da bra til med hjertehelsen spesielt og allmennhelsen generelt? Nei. Hvem er hardest rammet? Barn og ungdom. Hvorfor?
Det har blitt hevdet at klimaendringer er «vår tids største helsetrussel» (4). Stemmer det?
1. Bønaa KH, Halle KK, Govatsmark RES, Berge VB, Kiel IA, Sulo G, Kvåle R. Insidens og letalitet av akutt hjerteinfarkt i Norge 2013–21. Tidsskr Nor Legeforen 2024; 144. doi: 10.4045/tidsskr.24.0237
2. Strøm MS, Sveen KA, Raknes G, Slungård GF, Reistad SR. Dødsårsaksregisteret: Dødsårsaker i Norge 2023. Oslo: Folkehelseinstituttet, 2024. https://www.fhi.no/publ/2024/dodsarsaker-i-norge-2023/
3. Folkehelseinstituttet. Legemiddelstatistikk (2004-2023). https://statistikk.fhi.no/lmr/MWOZ5EnN09cSl9qpinD2mQ Lest 17.10.2024.
4. Kvåle G, Fadnes LT, Tryland M, Pihlstrøm L. Klimaendringer – vår tids største helsetrussel. Tidsskr Nor Legeforen 2011; 131. doi: 10.4045/tidsskr.11.0607