Main findings
The scoring system NEWS2 is suitable for detecting sepsis in ward patients.
Respiratory dysfunction led to a diagnosis of sepsis in most patients.
Sepsis is one of the most common causes of death in hospital, and at least one in eight patient deaths in hospital in Norway are from sepsis (1). Incidence increases with advancing age, and more cases of sepsis are expected in coming years due to the ageing population (2, 3). Rapid diagnosis and initiation of antibiotic treatment are the most important steps in severe infections (4). Early detection of sepsis has been a key area of focus for the Norwegian Board of Health Supervision, which conducted a nationwide inspection in 2016–2018 into the management of patients with sepsis in emergency departments (5). The inspection revealed a lack of prioritisation of resources for sepsis patients and delayed initiation of antibiotic treatment. However, the Board did not investigate the management of ward patients. It is also likely that nosocomial sepsis represents a considerable proportion of all cases of sepsis in hospitals, although data are sparse in this regard both at a national and international level (1, 3, 6).
Several scoring systems use vital signs to identify patients with sepsis or other causes of deterioration in a patient's condition. The SIRS (Systemic Inflammatory Response Syndrome) scoring system is a measure of the degree of inflammation and has been used in Norwegian hospitals since the late 1990s (7). The main weakness of the SIRS score is very low specificity in identifying sepsis (8, 9). Following the change in international guidelines in 2016, sepsis was defined as a dysregulated host response to infection leading to organ failure, and more specifically a rise in the SOFA (Sequential Organ Failure Assessment) score of 2 or more. SOFA is a comprehensive scoring system for the assessment of organ failure in six organs and was primarily developed for use in intensive care units. SOFA consists of a comprehensive evaluation of blood samples and clinical parameters, which is time-consuming and relatively resource-intensive, and it is less suitable for clinical use in emergency departments and on wards (8). Therefore, the qSOFA (quick Sequential Organ Failure Assessment) scoring system was launched at the same time to identify patients with sepsis outside intensive care units. This scoring system has high specificity, but low sensitivity (9–12). The Norwegian Directorate of Health has recommended that NEWS (National Early Warning Score) be used on wards in Norwegian hospitals for the detection of deterioration and sepsis (13). NEWS is not a scoring system specifically for infection, but rather a tool for the systematic monitoring of a patient's vital signs in order to detect changes in their condition (9). NEWS was updated in 2017 to take account of prior respiratory failure, among other things, and now the updated NEWS2 is mainly used. This scoring system has been reported to be better suited for the detection of sepsis than qSOFA and SIRS (9–11, 14). As far as we know, there has been no previous publication of a comparison of the scoring systems for sepsis diagnosis on wards in Norwegian hospitals, although international data are available (15).
The objective of this study was to investigate which of the scoring systems SIRS, qSOFA and NEWS2 were best suited for the early detection of sepsis on wards.
Material and method
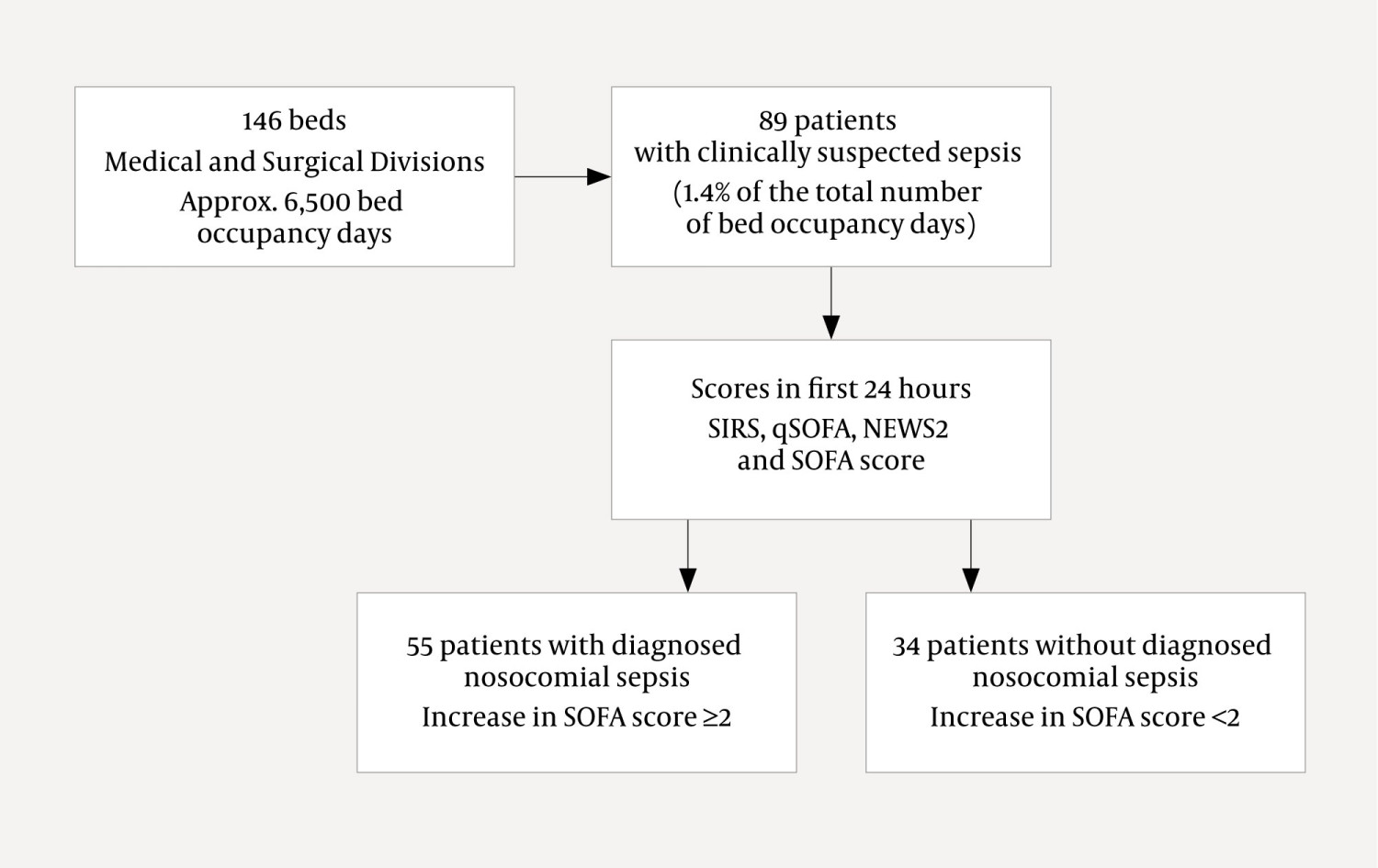
The project was a quality study conducted at Haukeland University Hospital in the period March–December 2019. The study was assessed by the Regional Committees for Medical and Health Research Ethics as a quality assurance project (REC West 2018/2535) and was notified to the data protection officer for Bergen Hospital Trust (PVO 00288), with no objections being raised. No data were collected other than data recorded routinely as part of workup and treatment, and therefore patient consent was not obtained. Adult patients over the age of 18 years from five medical and four surgical wards with a total of 146 beds were included. The Medical Division at Haukeland University Hospital has approximately 5,500 bed occupancy days per year, while the Surgical Division has approximately 8,500 per year.
Inclusion criteria were the clinical suspicion by a doctor treating an inpatient on the ward that the patient had new onset of severe infection (Figure 1). We included predominantly nosocomial infections discovered on the ward and not diagnosed on arrival at hospital. Patients with primarily community-acquired infection with deterioration after admission were also included. These patients had infection without sepsis on admission, but subsequently developed sepsis on the ward. The inclusion criteria were that the patient had an initial infection without sepsis for the first 24 hours and developed secondary deterioration more than 24 hours after admission. Identification of patients was carried out by two of the authors reviewing lists of inpatients on individual wards with a doctor or nurse, as well as mandatory review of medical documentation in electronic patient medical records. Identification of patients with suspected sepsis was supported if the attending doctor initiated or changed antibiotic treatment in addition to ordering new microbiological diagnostic tests, which is recommended in the latest sepsis definition for the identification of sepsis patients in studies (8). Comorbidities, age and sex were recorded based on electronic patient medical records. The suspected focus of infection was recorded from medical record notes and additional investigations for suspected severe infection, and verified in consultation with the departmental staff treating the patients.
Data from the electronic medical records system DIPS and the charting system Meona were recorded for 24 hours from the first moment that severe infection was suspected. Values that were recorded at the closest possible time to the suspicion of severe infection were used to score the patients in SIRS, qSOFA and NEWS2. For scoring in SOFA, values prior to suspicion of severe infection were compared with the worst single values measured in the next 24 hours (7, 8, 11). The SIRS criteria include two or more of the variables of temperature (> 38 °C or <36°C), pulse rate (> 90 bpm), respiratory rate (> 20 breaths per minute) and leukocyte count (> 12 × 109/L or <4 × 109/L). The qSOFA test was defined as positive if at least two of the following criteria were fulfilled: systolic blood pressure ≤ 100 mmHg, respiratory rate ≥ 22 breaths per minute and altered mental status. NEWS2 includes a number of parameters and is presented in Table 1. A NEWS2 score of ≥ 5 is considered the threshold, in addition to a value of 3 in any single vital parameter category (14).
Table 1
NEWS2 (National Early Warning Score 2). Scoring system based on six physiological parameters. The system takes account of pre-existing respiratory failure. Based on (14).
| Parameter | Score | ||||||
|---|---|---|---|---|---|---|---|
| 3 | 2 | 1 | 0 | 1 | 2 | 3 | |
| Respiratory rate (breaths per minute) | ≤ 8 | 9–11 | 12–20 | 21–24 | ≥ 25 | ||
| SpO2, scale 1 (%)1 | ≤ 91 | 92–93 | 94–95 | ≥ 96 | |||
| SpO2, scale 2 (%)1 | ≤ 83 | 84–85 | 86–87 | 88–92 | 93–94 on O2 | 95–96 on O2 | ≥ 97 on O2 |
| Room air or oxygen | oxygen | room air | |||||
| Systolic blood pressure (mmHg) | ≤ 90 | 91–100 | 101–110 | 111–219 | ≥ 220 | ||
| Pulse rate (bpm) | ≤ 40 | 41–50 | 51–90 | 91–110 | 111–130 | ≥ 131 | |
| Level of consciousness2 | A | C, V, P, U | |||||
| Temperature (°C) | ≤ 35.0 | 35.1–36.0 | 36.1–38.0 | 38.1–39.0 | ≥ 39.1 | ||
1SpO2 scale 2 should be reserved for patients with known hypercapnic respiratory failure with target SpO2 of 88–92 %, verified by blood gas analysis. The doctor should document in the medical records when scale 2 should be used. Scale 1 should be used in all other cases.
2Level of consciousness: A = alert, C = new confusion, V = responds to verbal stimulus, P = responds to pain stimulus, U = unresponsive to verbal or pain stimulus.
Sepsis was defined as infection and an increase in SOFA score of ≥ 2 in the first 24 hours after severe infection was suspected (8). The various parameters included in the SOFA score are presented in Table 2 (16). For 58 patients, the fraction of O2 was known in their treatment, but data from arterial blood gas analysis and thus arterial pressure of oxygen (PaO2) were missing. These patients' SOFA score for the respiratory system was estimated by using a published conversion table (17). The table was missing a threshold for a SOFA score of 1. We decided to use > 90 % oxygen saturation on room air as a threshold for a SOFA score of 1 based on previous practice at Haukeland University Hospital and other Norwegian hospitals (18). Bilirubin was the marker with most missing data (32 patients), which might result in underestimation of the SOFA score. Since previous studies have demonstrated a low incidence of hepatic failure with sepsis (2.4 %), the effect of this will probably be low (1). Medical records were reviewed two months after the end of the inclusion period to record 30-day mortality.
Table 2
SOFA (Sequential Organ Failure Assessment). Scoring system based on parameters from six organ systems (16). MAP = mean arterial pressure, GCS = Glasgow Coma Scale, DA = dopamine (μg/kg/min), DB = dobutamine (μg/kg/min), A = adrenaline (μg/kg/min), NA = noradrenaline (μg/kg/min).
| Organ system | Parameter | Score | ||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | ||
| Respiration | PaO2/FiO2 (kPa) | > 53.3 | <53.3 | <40 | <26.71 | <13.31 |
| Circulation | MAP (mmHg) | > 70 | <70 | DA <5 | DA 5.1–15 | DA > 15 |
| Central nervous system | GCS | 15 | 13–14 | 10–12 | 6–9 | <6 |
| Renal | Urine production (mL/24 hours) | <500 | <200 | |||
|
| Creatinine (µmol/L) | <110 | 110–170 | 171–299 | 300–440 | > 440 |
| Coagulation | Platelets (× 103/µL) | ≥ 150 | <150 | <100 | <50 | <20 |
| Hepatic | Bilirubin (µmol/L) | <20 | 20–32 | 33–101 | 102–204 | > 204 |
1With mechanical ventilation.
Statistics
Sensitivity, specificity, positive predictive value and negative predictive value for sepsis were calculated for each test. Statistical analysis included the Mann-Whitney test for comparison of continuous non-parametric data and the chi-squared test for comparison of categorical variables. A ROC (receiver operating characteristic) curve was plotted for each test, including Youden's index, using GraphPad Prism 8 (GraphPad Software, San Diego, California, USA). MedCalc version 20.109 (MedCalc Software bv, Ostend, Belgium) was used for pairwise comparison of the area under the ROC curve with DeLong's test. Calculation of statistical power for mortality prediction found that 200 patients needed to be included to provide sufficient power to be able to demonstrate the scoring systems' ability to predict mortality. Unfortunately, resources were not available for further patient inclusion in this project, but we have nevertheless decided to publish the data.
Results
A total of 89 patients with suspected sepsis were included in the study. The most common suspected focus of infection was the abdomen (28 patients, 31 %), respiratory tract (21 patients, 24 %) and urinary tract (9 patients, 10 %). No definite focus of infection was detected in 24 patients (28 %). The main clinical data are presented in Table 3. The criteria for sepsis with an increase in SOFA score of ≥ 2 were fulfilled in 55 patients (62 %). Respiratory dysfunction led to the diagnosis of sepsis in most of the patients, and 51 (93 %) of the 55 patients with an increase in SOFA score of ≥ 2 were allocated points in this category. The next most common organ failure was circulatory failure, which was recorded in 26 patients (47 %). All of the 9 patients who died within 30 days of inclusion had been diagnosed with sepsis, which corresponds to a mortality rate in the sepsis group of 16 % (9 out of 55).
Table 3
Data for 89 patients with clinical suspicion of sepsis at Haukeland University Hospital. In the 'Sepsis' and 'Not sepsis' columns, the figures state the number (%) unless otherwise specified. Significant p-values are shown in bold. qSOFA = quick Sequential Organ Failure Assessment, SIRS = Systemic Inflammatory Response Syndrome, NEWS2 = National Early Warning Score 2.
| Variable | Sepsis | Not sepsis | p-value | |
|---|---|---|---|---|
| Age in years, median (distribution) | 67 (21–75) | 60 (20–91) | 0.066 | |
| Female | 23 (42) | 13 (38) | 0.738 | |
| Comorbidities |
|
|
| |
|
| At least one comorbidity | 38 (69) | 28 (82) | 0.165 |
|
| Hypertension | 19 (35) | 5 (15) | 0.040 |
|
| Cardiovascular disease | 20 (36) | 5 (15) | 0.027 |
|
| Chronic pulmonary disease | 3 (5) | 2 (6) | 0.932 |
|
| Chronic kidney disease | 5 (9) | 3 (9) | 0.965 |
|
| Hepatic failure | 3 (5) | 0 (0) | 0.166 |
|
| Diabetes | 12 (22) | 5 (15) | 0.407 |
|
| Immunosuppression | 7 (13) | 15 (35) | 0.001 |
|
| Malignancy | 16 (29) | 20 (59) | 0.006 |
| Suspected focus of infection |
|
|
| |
|
| Abdomen | 19 (35) | 9 (26) | 0.425 |
|
| Respiratory tract | 11 (20) | 10 (29) | 0.310 |
|
| Urinary tract | 7 (13) | 2 (6) | 0.298 |
|
| Soft tissue | 5 (9) | 2 (6) | 0.585 |
|
| Unknown | 13 (24) | 11 (32) | 0.368 |
| Ward |
|
|
| |
|
| Medical | 21 (38) | 26 (76) | <0.001 |
|
| Surgical | 34 (62) | 8 (24) | <0.001 |
| Bacteriaemia | 14 (25) | 6 (11) | 0.391 | |
| Clinical variables, median (distribution) |
|
|
| |
|
| Respiratory rate, breaths per minute | 22 (12–44) | 24 (15–37) | 0.452 |
|
| SpO2, % | 93 (62–98) | 94 (90–100) | 0.002 |
|
| Systolic blood pressure, mmHg | 125 (65–185) | 133 (92–202) | 0.076 |
|
| Pulse rate, bpm | 102 (60–142) | 109 (71–147) | 0.094 |
|
| Temperature, °C | 38.1 (35.9–40.9) | 38.4 (37.3–39.5) | 0.023 |
|
| Leukocytes, × 109/L | 10.5 (0.2–94.4) | 8.9 (0.2–19.9) | 0.319 |
| Scoring system, median (distribution)1 |
|
|
| |
|
| qSOFA | 1 (0–2) | 0 (0–2) | <0.001 |
|
| SIRS | 3 (0–4) | 3 (1–4) | 0.141 |
|
| NEWS2 | 7 (2–12) | 4 (1–10) | <0.001 |
|
| SOFA | 3 (2–10) | 1 (0–5) | <0.001 |
| Mortality | 9 (16) | 0 | 0.013 | |
1Values recorded as close as possible to the time that severe infection was suspected were used to score the patients on qSOFA, SIRS and NEWS2. For scoring on SOFA, values prior to suspicion of severe infection were compared with the worst single values measured in the following 24 hours.
The three scoring systems are presented in Table 4. System characteristics in the detection of sepsis are presented in Table 5. ROC analysis was performed to investigate the ability of the various scoring systems to identify patients with sepsis (Figure 2). Increasing area under the curve (AUC) represents the test's increasing ability to diagnose the condition – an ideal test would have an area of 1.0. For NEWS2, we found an AUC value of 0.79 (95 % CI 0.69 to 0.87), while it was lower for both qSOFA and SIRS, which had AUC values of 0.74 (95 % CI 0.63 to 0.82) and 0.59 (95 % CI 0.48 to 0.69) respectively. There was a significant difference between the AUC value for NEWS2 and SIRS (p = 0.03), while the AUC value for qSOFA was not significantly different from the values for NEWS2 and SIRS.
Table 4
Results for the various scoring systems for patients with and without sepsis at Haukeland University Hospital, stated as number of patients (%) in each group. qSOFA = quick Sequential Organ Failure Assessment, SIRS = Systemic Inflammatory Response Syndrome, NEWS2 = National Early Warning Score 2.
| Scoring system | Sepsis | Not sepsis | Total | |
|---|---|---|---|---|
| qSOFA |
|
|
| |
|
| ≥ 2 | 11 (20) | 1 (3) | 12 (13) |
|
| <2 | 44 (80) | 33 (97) | 77 (87) |
| SIRS |
|
|
| |
|
| ≥ 2 | 45 (82) | 32 (94) | 77 (87) |
|
| <2 | 10 (18) | 2 (6) | 12 (13) |
| NEWS2 |
|
|
| |
|
| ≥ 5 in total and/or 3 in a single parameter | 53 (96) | 14 (41) | 67 (75) |
|
| <5 in total and/or < 3 in all parameters | 2 (4) | 20 (59) | 22 (25) |
|
| ≥ 5 | 51 (93) | 13 (38) | 64 (72) |
|
| <5 | 4 (7) | 21 (62) | 25 (28) |
Table 5
Test characteristics in the detection of sepsis with established thresholds for qSOFA, SIRS and NEWS2 in patients with clinically suspected sepsis at Haukeland University Hospital. Values are stated as percentages with 95 % confidence interval (CI). Please note that NEWS2 can also be used with an alert threshold of a score of 3 in a single parameter. qSOFA = quick Sequential Organ Failure Assessment, SIRS = Systemic Inflammatory Response Syndrome, NEWS2 = National Early Warning Score 2.
| Variable | qSOFA ≥ 2 (95 % CI) | SIRS ≥ 2 (95 % CI) | NEWS2 ≥ 5 in total and/or 3 in a single parameter (95 % CI) | NEWS2 ≥ 5 (95 % CI) |
|---|---|---|---|---|
| Sensitivity | 20 (12 to 32) | 82 (70 to 90) | 96 (88 to 99) | 93 (83 to 97) |
| Specificity | 97 (85 to 100) | 6 (1 to 19) | 59 (42 to 74) | 62 (45 to 76) |
| Positive predictive value | 92 (65 to 100) | 58 (47 to 69) | 79 (68 to 87) | 80 (68 to 88) |
| Negative predictive value | 43 (32 to 54) | 17 (3 to 45) | 91 (72 to 98) | 84 (65 to 94) |
| Mortality rate | 8 | 8 | 13 | 14 |
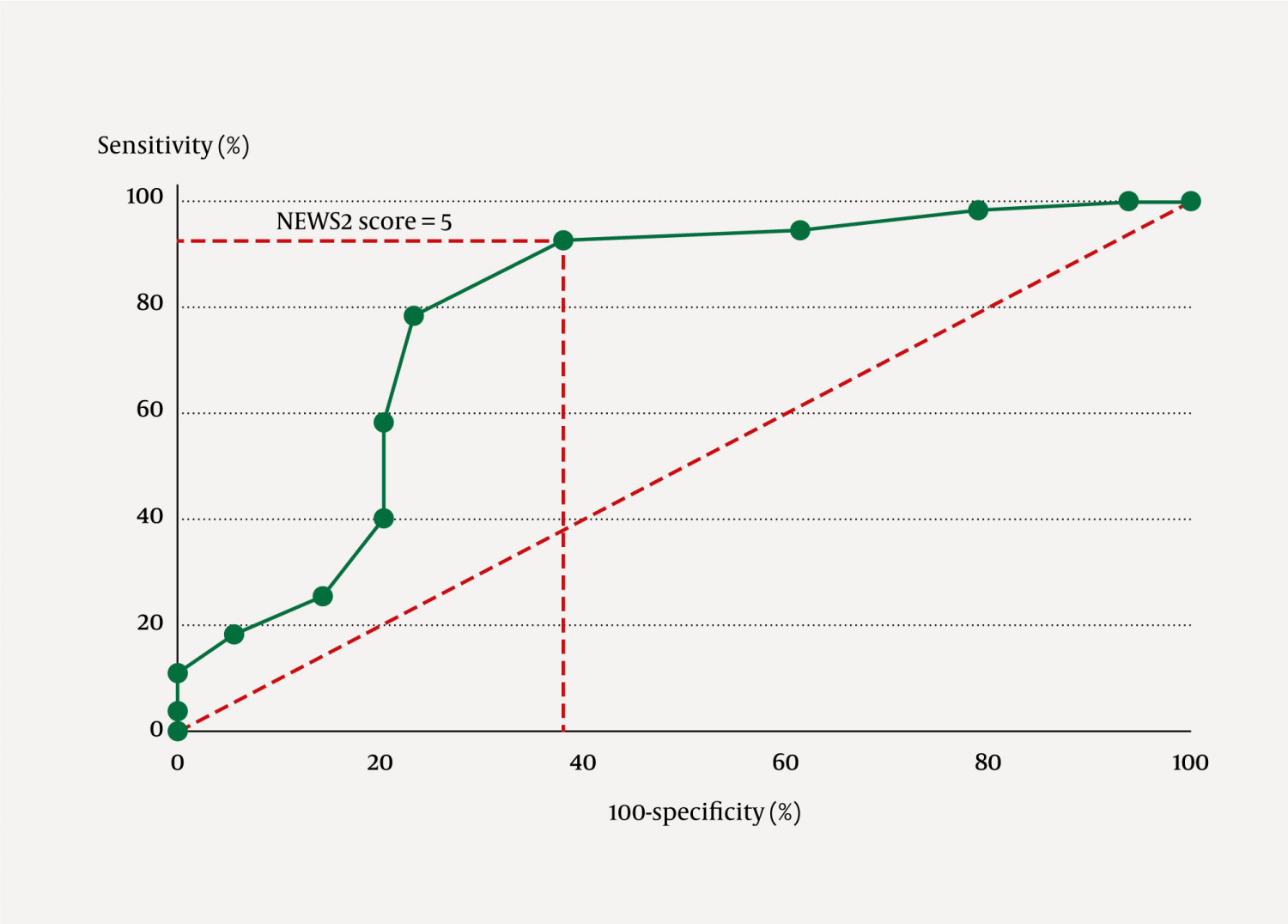
The best threshold for detection of sepsis with the various tests was investigated with Youden's index, which tests for the best statistical threshold regardless of its clinical relevance because high sensitivity and negative predictive value are often more important. The results differed somewhat from established thresholds, with a best threshold of 6 for NEWS2 with a sensitivity of 78 % and specificity of 76 %, and ≥ 2 for qSOFA with a sensitivity of 20 % and specificity of 97 %. The best threshold for SIRS was difficult to evaluate since more of the patients without sepsis fulfilled four SIRS criteria, so there is little clinical relevance in presenting Youden's index values for SIRS.
To establish the possible reason for the differences in detection of sepsis by the various scoring systems, we evaluated the test characteristics for the individual parameters. Out of the parameters recorded, the most sensitive measure of sepsis was oxygen saturation with a threshold of 95 % (85 %). We also found a correlation between respiratory rate and decreasing oxygen saturation (r = −0.30, p = 0.017). Pulse rate > 100 bpm had a sensitivity of 71 %. The remaining parameters had a sensitivity of between 18 % and 55 %, with the GCS (Glasgow Coma Scale) parameter having the lowest. We recorded ten patients with altered mental status, all of whom were diagnosed with sepsis. The most specific parameters were altered mental status (measured with GCS score) and decreased systolic blood pressure, followed by oxygen saturation.
Discussion
NEWS2 was the most sensitive scoring system in identifying patients with sepsis on wards, while qSOFA had the highest specificity. The AUC values were acceptable for both NEWS2 and qSOFA, but the low sensitivity of qSOFA entails a high risk of missing most cases of sepsis if this system is used alone.
Although few of the ward patients with sepsis were included in this study, the results are consistent with previous studies conducted in emergency departments (9–11). It has largely been demonstrated that NEWS2 is able to predict mortality and need for intensive care treatment for both patients in emergency departments and those on wards (15, 19), but the statistical power of our study was too low to draw any conclusions about whether NEWS2 predicts mortality. Two Norwegian studies have found that NEWS2 was also useful in predicting outcomes in COVID-19 patients (20, 21).
In the Norwegian Board of Health Supervision's assessment of sepsis treatment, the main concern was a lack of prioritisation of resources for sepsis patients in emergency departments (5). A lack of specificity of SIRS and hence an inability to prioritise was also the reason for international guidelines recommending a move away from the SIRS criteria in the sepsis definition in 2016 (8). In 2021, the Surviving Sepsis Campaign (SSC) published updated guidelines warning against the use of qSOFA alone as a scoring system to detect sepsis because its sensitivity is too low, which is in line with our results (22).
The best thresholds for detection of sepsis in our study according to statistical analysis with Youden's index were 6 for NEWS2 and 4 for SIRS. This differs from the established thresholds of 5 and 2 respectively. Our assessment is that the established thresholds provide better sensitivity, but that NEWS2 with a threshold of 5 still has acceptable specificity. Tables 4 and 5 show little difference in sensitivity and specificity with NEWS2 if a score of 3 in a single parameter is included in addition to an aggregate score of 5 as a threshold, which was the initial recommendation for NEWS2 (14). There are similar findings in a study, i.e. that it would be sufficient to keep an aggregate score of 5 alone as the threshold for NEWS2 because the addition of one single parameter of 3 would create an increased burden of work without any great improvement in sensitivity (23). Therefore, in the latest version of NEWS2, the National Health Service (NHS) recommends giving patients with a single parameter score of 3 closer monitoring and assessment on the ward, but not the same alerting of doctors as a total NEWS2 score of 5 or more (14).
There are several weaknesses with the study. The inclusion criterion was a clinical suspicion on the part of clinical staff treating a ward inpatient that the patient had a severe infection. However, we did not record data from all inpatients on wards in the inclusion period because our electronic medical records systems were not equipped for that type of data collection. Although inpatients were assessed for all days in the inclusion period, we cannot rule out the fact that individual patients with suspected severe infection were not included in the study. An important weakness is that the assessment of the focus of infection was based on the subjective diagnosis of the clinician treating the patient, and that no post-hoc assessment of the probability of infection was performed (24). However, the main weakness was that too few patients were included in the study to be able to assess the scoring systems' ability to predict mortality since it has previously been demonstrated that NEWS2 can be used for this purpose (15).
Clinical parameters were recorded in cases of clinical suspicion of infection. Since the study was partly based on a retrospective review of data collected from patient medical records, it has been challenging to obtain complete data, and data are missing for several patients. Oxygen saturation was the most sensitive single parameter for sepsis, while at the same time it was also the most problematic to interpret. The most challenging aspect of calculating the total SOFA score was calculating the SOFA score for respiration in patients for whom arterial blood gas analysis results were missing. We identified the best estimated value using a table to impute a ratio calculated from oxygen saturation, but discovered early on that this had its limitations (9, 17). The table does not give definite values for a SOFA score of 1, and the fact that we had to use thresholds previously used for respiratory failure in sepsis resulted in uncertainty in the recording of respiratory failure. If we only recorded those patients for whom arterial blood gas results were available, the proportion with recorded respiratory failure would have been underestimated. If we had followed the table without correction, the proportion with respiratory failure would have been overestimated. Another option for calculating a SOFA score based on peripheral oxygen saturation may be to use oxygen saturation of 94 % and 91 % on room air as thresholds for SOFA scores of 1 and 2 respectively, which has recently been proposed and validated in a larger patient cohort (25).
The assessment of mental status is also challenging. A large proportion of altered mental status in this study was recorded by nurses who used NEWS2 for scoring. However, there is a risk that this value is underestimated because a systematic screening tool, for example 4AT, was not used to record altered mental status (26).
Prompt antibiotic treatment is the single measure that has greatest impact for the prognosis of sepsis patients (5). Data from Norway demonstrate that early detection of sepsis on the ward results in reduced mortality (27). Deterioration in a patient's condition often occurs gradually, and it is important to detect changes early enough to prevent the development of sepsis and organ failure. In this study, we found that reduced oxygen saturation was more sensitive than other parameters such as mental status, which may help explain differences between the various scoring systems.
Conclusion
Our data indicate that NEWS2 is better suited than qSOFA and SIRS to detect sepsis in patients on the wards.
Steinar Skrede and Knut Anders Mosevoll received research grants from the Research Council of Norway via NordForsk (project number 90456), ERA PerMed (project 2018 - 151, PerMIT) and the Swedish Research Council (project number 2018 - 02475).
The article has been peer-reviewed.
- 1.
Knoop ST, Skrede S, Langeland N et al. Epidemiology and impact on all-cause mortality of sepsis in Norwegian hospitals: A national retrospective study. PLoS One 2017; 12: e0187990. [PubMed][CrossRef]
- 2.
Flaatten H. Epidemiology of sepsis in Norway in 1999. Crit Care 2004; 8: R180–4. [PubMed][CrossRef]
- 3.
Rudd KE, Johnson SC, Agesa KM et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet 2020; 395: 200–11. [PubMed][CrossRef]
- 4.
Seymour CW, Gesten F, Prescott HC et al. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis. N Engl J Med 2017; 376: 2235–44. [PubMed][CrossRef]
- 5.
Helsetilsynet. Sepsis – ingen tid å miste. Oppsummering av landsomfattende tilsyn i 2016–2018 med spesialisthelsetjenesten:helseforetakenes somatiske akuttmottak og deres identifisering og behandling av pasienter med sepsis. Oslo: Helsetilsynet, 2018.
- 6.
Eriksen HM, Iversen BG, Aavitsland P. Prevalence of nosocomial infections in hospitals in Norway, 2002 and 2003. J Hosp Infect 2005; 60: 40–5. [PubMed][CrossRef]
- 7.
Bone RC, Balk RA, Cerra FB et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992; 101: 1644–55. [PubMed][CrossRef]
- 8.
Singer M, Deutschman CS, Seymour CW et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315: 801–10. [PubMed][CrossRef]
- 9.
Usman OA, Usman AA, Ward MA. Comparison of SIRS, qSOFA, and NEWS for the early identification of sepsis in the Emergency Department. Am J Emerg Med 2019; 37: 1490–7. [PubMed][CrossRef]
- 10.
Goulden R, Hoyle MC, Monis J et al. qSOFA, SIRS and NEWS for predicting inhospital mortality and ICU admission in emergency admissions treated as sepsis. Emerg Med J 2018; 35: 345–9. [PubMed][CrossRef]
- 11.
Inada-Kim M, Nsutebu E. NEWS 2: an opportunity to standardise the management of deterioration and sepsis. BMJ 2018; 360: k1260. [PubMed][CrossRef]
- 12.
Askim Å, Moser F, Gustad LT et al. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality - a prospective study of patients admitted with infection to the emergency department. Scand J Trauma Resusc Emerg Med 2017; 25: 56. [PubMed][CrossRef]
- 13.
Helsedirektoratet. Tidlig oppdagelse og rask respons ved forverret somatisk tilstand. Oslo: Helsedirektoratet, 2020. https://www.helsedirektoratet.no/faglige-rad/tidlig-oppdagelse-og-rask-respons-ved-forverret-somatisk-tilstand Accessed 16.11.2022.
- 14.
Royal College of Physicians. National Early Warning Score (NEWS) 2: Standardising the assessment of acute-illness severity in the NHS. Updated report of a working party. London: RCP, 2017. https://www.rcplondon.ac.uk/projects/outputs/national-earlywarning-score-news-2 Accessed 5.12.2022.
- 15.
Fernando SM, Fox-Robichaud AE, Rochwerg B et al. Prognostic accuracy of the Hamilton Early Warning Score (HEWS) and the National Early Warning Score 2 (NEWS2) among hospitalized patients assessed by a rapid response team. Crit Care 2019; 23: 60. [PubMed][CrossRef]
- 16.
Lambden S, Laterre PF, Levy MM et al. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit Care 2019; 23: 374. [PubMed][CrossRef]
- 17.
Pandharipande PP, Shintani AK, Hagerman HE et al. Derivation and validation of Spo2/Fio2 ratio to impute for Pao2/Fio2 ratio in the respiratory component of the Sequential Organ Failure Assessment score. Crit Care Med 2009; 37: 1317–21. [PubMed][CrossRef]
- 18.
Norsk Legemiddelhåndbok. T1.10 Sepsis. https://www.legemiddelhandboka.no/T1.10/Sepsis Accessed 5.12.2022.
- 19.
Engebretsen S, Bogstrand ST, Jacobsen D et al. NEWS2 versus a single-parameter system to identify critically ill medical patients in the emergency department. Resusc Plus 2020; 3: 100020. [PubMed][CrossRef]
- 20.
Holten AR, Nore KG, Tveiten CEVWK et al. Predicting severe COVID-19 in the Emergency Department. Resusc Plus 2020; 4: 100042. [PubMed][CrossRef]
- 21.
Myrstad M, Ihle-Hansen H, Tveita AA et al. National Early Warning Score 2 (NEWS2) on admission predicts severe disease and in-hospital mortality from Covid-19 - a prospective cohort study. Scand J Trauma Resusc Emerg Med 2020; 28: 66. [PubMed][CrossRef]
- 22.
Evans L, Rhodes A, Alhazzani W et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit Care Med 2021; 49: e1063–143. [PubMed][CrossRef]
- 23.
Jarvis S, Kovacs C, Briggs J et al. Aggregate National Early Warning Score (NEWS) values are more important than high scores for a single vital signs parameter for discriminating the risk of adverse outcomes. Resuscitation 2015; 87: 75–80. [PubMed][CrossRef]
- 24.
Madsen MB, Skrede S, Perner A et al. Patient's characteristics and outcomes in necrotising soft-tissue infections: results from a Scandinavian, multicentre, prospective cohort study. Intensive Care Med 2019; 45: 1241–51. [PubMed][CrossRef]
- 25.
Valik JK, Mellhammar L, Sundén-Cullberg J et al. Peripheral Oxygen Saturation Facilitates Assessment of Respiratory Dysfunction in the Sequential Organ Failure Assessment Score With Implications for the Sepsis-3 Criteria. Crit Care Med 2022; 50: e272–83. [PubMed]
- 26.
Myrstad M, Kuwelker K, Haakonsen S et al. Delirium screening with 4AT in patients aged 65 years and older admitted to the Emergency Department with suspected sepsis: a prospective cohort study. Eur Geriatr Med 2022; 13: 155–62. [PubMed][CrossRef]
- 27.
Torsvik M, Gustad LT, Mehl A et al. Early identification of sepsis in hospital inpatients by ward nurses increases 30-day survival. Crit Care 2016; 20: 244. [PubMed][CrossRef]