Subacute thyroiditis was identified through histological examination of the right thyroid lobe, removed in connection with treatment of a young woman for thyroid carcinoma. She had received an mRNA vaccination against SARS-CoV-2 six days previously.
A previously mainly healthy woman in her thirties was referred for an ultrasound scan after discovering a lump on her throat. An ultrasound scan revealed changes characteristic of thyroiditis and a hypoechoic nodule measuring 7 x 13 mm in the left lobe. The left thyroid lobe was extirpated after a cytological examination of fine-needle aspirate from the nodule revealed papillary thyroid carcinoma (not shown).
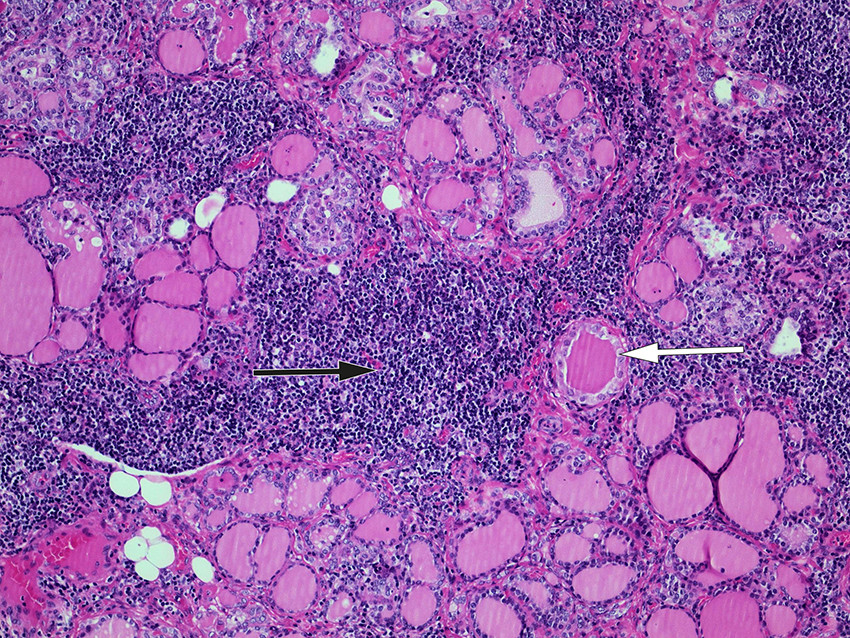
The procedure and post-operative course were without complications. On analysis, thyroid function markers showed an elevated value for antibodies against thyroid peroxidase (anti-TPO) of 623 kIU/L (reference range < 35), a finding associated with Hashimoto's thyroiditis. Thyroid-stimulating hormone (P-TSH) varied within the range 3.2–4.7 mIU/L (0.35–3.6), and P-fT4 (tetraiodothyronine) varied within the range 9.5–13 pmol/L (9–19). This was consistent with latent hypothyroidism. A histological examination confirmed a papillary carcinoma (not shown) and Hashimoto's thyroiditis (Figure 1).
The patient was put on levothyroxine therapy. After an interdisciplinary assessment, a complementary hemithyroidectomy was recommended prior to radioactive iodine therapy. Three months after the first procedure, and six days before unilateral complementary lobectomy of the right lobe, the patient received her first dose of the Pfizer/BioNTech vaccine against the SARS-CoV-2 virus. Preoperatively, P-TSH was 20 mIU/L (0.35–3.6 × 10−3), PfT4 10 pmol/L (9–19), and sedimentation rate 6 mm/h (1–17).
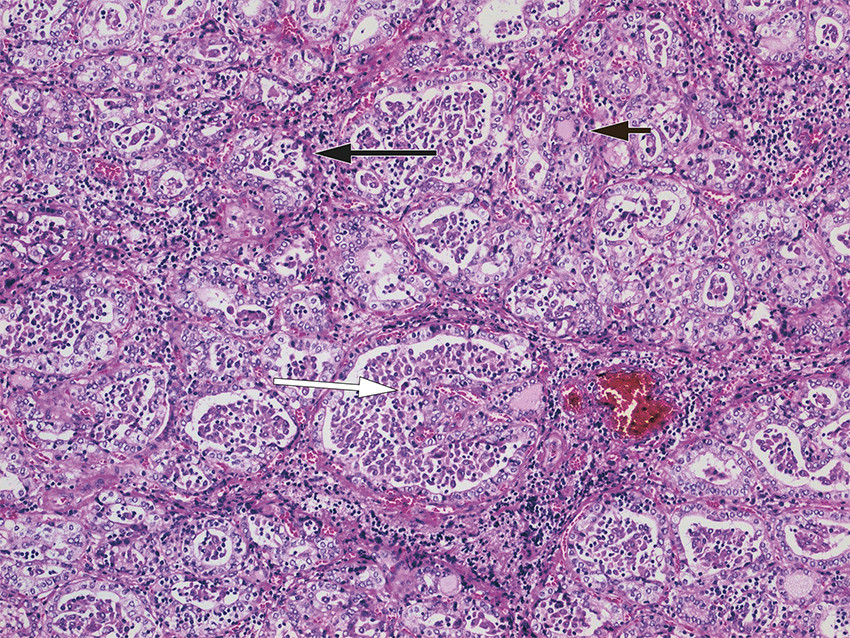
The description of the procedure indicated peroperative findings consistent with thyroiditis and fibrosis. The surgery took place without complications. A histological examination revealed changes consistent with subacute thyroiditis (Figure 2), but no evidence of a malignant tumour.
The patient was not aware of having had any COVID-19 infection, and there were no symptoms or biochemical findings to indicate a recently experienced or ongoing infection with other aetiology.
Discussion
Subacute thyroiditis is assumed to be associated with viral infections of the upper respiratory tract. Several virus types have been postulated as possible triggering agents (1, 2). A recently published case study in the Journal of the Norwegian Medical Association (3) described the onset of autoimmune thyroiditis in a patient who had been found to be infected with COVID-19 three weeks previously. A causal relationship between the COVID-19 infection and the autoimmune thyroiditis was regarded as probable.
Women are more susceptible to subacute thyroiditis than men. Patients normally experience low-grade fever, lethargy and a sore throat in the initial phase of the disease (4). As a rule, the diagnosis is made on the basis of typical clinical findings and laboratory tests, but an ultrasound scan and fine-needle aspirate may contribute to the diagnosis. A diagnosis is only in exceptional cases made on the basis of a post-operative tissue specimen. In the early phase, the histology picture is usually dominated by destroyed follicles with loss of epithelium and colloid. The picture gradually becomes granulomatous, with an increasing number of macrophages. There is an inadequate evidence base for deciding whether the development of the possibly vaccine-triggered histological changes follow the same course as changes triggered by an infectious disease. Sarcoidosis, palpation thyroiditis and other forms of granulomatous thyroiditis are all differential histological diagnoses for subacute thyroiditis, but none of these usually displays changes as pronounced as in the specimen in question.
Subacute thyroiditis has been described after vaccination with inactivated viral vaccines for seasonal influenza (5). A recently published case report describes subacute thyroiditis with onset five days after an mRNA SARS-CoV-2 vaccination (Pfizer/BioNTech) (6). Three cases have also been reported of subacute thyroiditis with onset 4–7 days after vaccination with inactivated SARS-CoV-2 (Coronavac) (7).
In the case report in question, histological changes typical of subacute thyroiditis were detected six days after an mRNA vaccine against SARS-CoV-2. The clinical records contained no information indicating that the patient had had or currently had a viral infection. The patient was not taking any drugs other than levothyroxine. A re-examination of the histological sections from the left thyroid lobe could not confirm subacute thyroiditis in this lobe, which indicates that the changes occurred in the time between the two procedures. As far as we know, earlier surgical procedures on the throat do not make patients susceptible to subacute thyroiditis. The same applies to treatment with levothyroxine. The morphology of the specimen in question revealed an inflammation that was more pronounced than in palpation thyroiditis, and without the well developed granulomas that would be expected with sarcoidosis.
In the absence of other known risk factors, in view of onset a short while after vaccination with an mRNA vaccine against SARS-CoV-2, and in light of the literature, we find it likely that the patient in this case report may have developed subacute thyroiditis as a result of vaccination. It is not possible either clinically or histologically to confirm with certainty that cases of subacute thyroiditis are triggered by an mRNA vaccine against SARS-CoV-2, but there is a possible causal relationship.
The patient has consented to the publication of the article. The article has been peer-reviewed.
- 1.
Desailloud R, Hober D. Viruses and thyroiditis: an update. Virol J 2009; 6: 5. [PubMed][CrossRef]
- 2.
Michas G, Alevetsovitis G, Andrikou I et al. De Quervain thyroiditis in the course of H1N1 influenza infection. Hippokratia 2014; 18: 86–7. [PubMed]
- 3.
Tjønnfjord E, Moe RB, Ghanima W et al. Subakutt tyreoiditt etter covid-19. Tidsskr Nor Legeforen 2021; 141. doi: 10.4045/ tidsskr.21.0169. [PubMed][CrossRef]
- 4.
Benbassat CA, Olchovsky D, Tsvetov G et al. Subacute thyroiditis: clinical characteristics and treatment outcome in fifty-six consecutive patients diagnosed between 1999 and 2005. J Endocrinol Invest 2007; 30: 631–5. [PubMed][CrossRef]
- 5.
Altay FA, Güz G, Altay M. Subacute thyroiditis following seasonal influenza vaccination. Hum Vaccin Immunother 2016; 12: 1033–4. [PubMed][CrossRef]
- 6.
Franquemont S, Galvez J. Subacute Thyroiditis After mRNA Vaccine for Covid-19. J Endocr Soc 2021; 5 (Suppl 1): A956–7. [CrossRef]
- 7.
İremli BG, Şendur SN, Ünlütürk U. Three Cases of Subacute Thyroiditis Following SARS-CoV-2 Vaccine: Postvaccination ASIA Syndrome. J Clin Endocrinol Metab 2021; 106: 2600–5. [PubMed][CrossRef]