Main findings
Prescribing practices for clozapine vary considerably between different counties
Oslo, Akershus and Rogaland counties have a lower prescribing rate than the national average
Nordland, Troms and Sør-Trøndelag counties stand out in having a higher prescribing rate
Clozapine is considered to be the most effective antipsychotic drug for treatment of schizophrenia (1). However, because of serious adverse effects, such as agranulocytosis, this is not a first-line drug. The Norwegian national guidelines for examination, treatment and follow-up of persons with psychotic disorders recommend that patients with treatment-resistant schizophrenia, defined as two failed treatment attempts with other antipsychotic drugs, be offered treatment with clozapine (2). This recommendation accords with international guidelines (3–5).
Despite these consistent international guidelines there is considerable variation in the use of clozapine between nations with comparable populations. For example, in 2014 this drug was prescribed to 50 per 100 000 inhabitants in Norway, compared to 58, 61, 100 and 189 per 100 000 inhabitants in Denmark, Sweden, Iceland and Finland respectively (6). The prevalence of schizophrenia may also vary (7, 8) and thus possibly represent a partial explanation for the variations in the use of clozapine between nations. On the other hand, studies show that clozapine is used more rarely (9–11) and later (12) than recommended, even when an indication is evident.
Patient pathways for examination and treatment in the mental health services for adults were implemented in Norway on 1 January 2019 (13). One of the five objectives of these patient pathways is to provide 'an equal service to patients [...] irrespective of where in the country they live'. A study of geographical variation in the prescribing rate for clozapine may give an indication of the extent to which patients with treatment-resistant schizophrenia are provided with drug-based treatment of equal quality.
The main goal of this study was to investigate the extent to which the prescribing rate for clozapine varied between Norwegian counties in 2016. The first objective was to investigate whether this variation could be explained in terms of differences in the proportion of patients with schizophrenia who were followed up by the specialist health services in the different counties. The second objective was to describe the differences in prescribing rates between the country's four regional health authorities among men and women in different age groups. The third objective was to investigate whether the differences in prescribing practices for clozapine between the country's four regional health authorities could be explained by varying prescribing rates for antipsychotic drugs as a group.
Material and method
This ecological study investigated the prescribing of clozapine for Norwegian counties and regional health authorities. The data material was retrieved from the Norwegian Prescription Database (14), the Norwegian Patient Registry and Statistics Norway. Since the data stem from the time when Norway had 19 counties, the old county names are used.
The Norwegian Prescription Database
The Norwegian Prescription Database contains aggregated data for all prescriptions dispensed by Norwegian pharmacies (reseptregisteret.no). Prescribing in hospitals and nursing homes is not included. We retrieved data for prescriptions of clozapine (ATC code N05AH02) for the year 2016 nationwide, distributed by counties and regional health authorities, sex and the age groups 20–29, 30–39, 40–49, 50–59 and 60–69 years. We used regional health authorities as the basis for examining the prescribing of clozapine to different sexes and age groups, because the figures for some counties were too small to retrieve aggregated data.
In the Norwegian Prescription Database, the clozapine dose is stated in terms of defined daily doses (DDD). This is an expression of the assumed average daily dose for adults, used for the main indication of the drug (300 mg for clozapine) (15). We investigated 1) the prescribing rate for clozapine (the number of persons with at least one prescription for clozapine during the year in question per 100 000 inhabitants), 2) the average prescribed clozapine dose per user (calculated as the number of DDDs per year divided by 365 and the number of users, reported in mg) and 3) the proportion of prescriptions for antipsychotic drugs (ATC N05A, excluding lithium (N05AN01)) that were accounted for by clozapine.
The Norwegian Patient Registry
Data for the number of patients diagnosed with schizophrenia (ICD-10 F20.0-F20.9) were retrieved from the Norwegian Patient Registry, which records diagnoses for all patient contacts in the specialist health services. We were provided with data on the number of patients over the age of 18 who were recorded with schizophrenia as their primary or secondary diagnosis following contact with the specialist health services (mental health care, interdisciplinary specialised addiction therapy or contract specialists in psychiatry) in 2016, by county.
Statistics Norway
Population figures (> 18 years) by county were retrieved from Statistics Norway for the same period. The proportion of the population that was followed up by the specialist health services because of a schizophrenia diagnosis was calculated by dividing the number of patients with this diagnosis with the number of inhabitants for each county. This should not be regarded as an estimate of prevalence, but as the proportion of the population that has contact with the specialist health services due to a diagnosis of schizophrenia.
Statistical methods
The estimation of a 95 % confidence interval (CI) for the prescribing rates for counties, regional health authorities, sexes and age groups was made according to the formula ![]() , where p is the proportion prescribed with clozapine and n is the number of individuals in the whole population (16). A confidence interval for the average clozapine dose prescribed cannot be estimated on the basis of aggregated data without a measure of dispersion. In light of the literature appendix), we assumed a standard deviation (SD) of 190 mg clozapine in the estimation of a 95 % confidence interval. The CI was subsequently estimated according to the formula for mean
, where p is the proportion prescribed with clozapine and n is the number of individuals in the whole population (16). A confidence interval for the average clozapine dose prescribed cannot be estimated on the basis of aggregated data without a measure of dispersion. In light of the literature appendix), we assumed a standard deviation (SD) of 190 mg clozapine in the estimation of a 95 % confidence interval. The CI was subsequently estimated according to the formula for mean ![]() , where n is the number of individuals who use clozapine ((16). Spearman's correlation coefficient was used to investigate possible correlations between the number of patients with a diagnosis of schizophrenia and the prescribing rate. The statistical significance level was set at 0.05. SPSS version 24 was used to perform the statistical analyses.
, where n is the number of individuals who use clozapine ((16). Spearman's correlation coefficient was used to investigate possible correlations between the number of patients with a diagnosis of schizophrenia and the prescribing rate. The statistical significance level was set at 0.05. SPSS version 24 was used to perform the statistical analyses.
Ethics
The study used aggregated data that are openly available online from the Norwegian Prescription Database and Statistics Norway. The data from the Norwegian Patient Registry were also aggregated information which is supplied for specific purposes without an application to the Regional Committee for Medical and Health Research Ethics.
Results
Prescribing in Norwegian counties
In Norway, 50 (95 % CI 48–52) per 100 000 inhabitants were dispensed a prescription for clozapine in 2016. The prescribing rate varied between counties from 38 (95 % CI 33–43) to 76 (95 % CI 63–89) per 100 000 inhabitants (Figure 1 and Table 1). Nordland, Sør-Trøndelag and Troms counties stood out in having the highest prescribing rate (> 70 per 100 000 inhabitants), while Oslo and Akershus counties had the lowest prescribing rates (< 40 per 100 000 inhabitants).
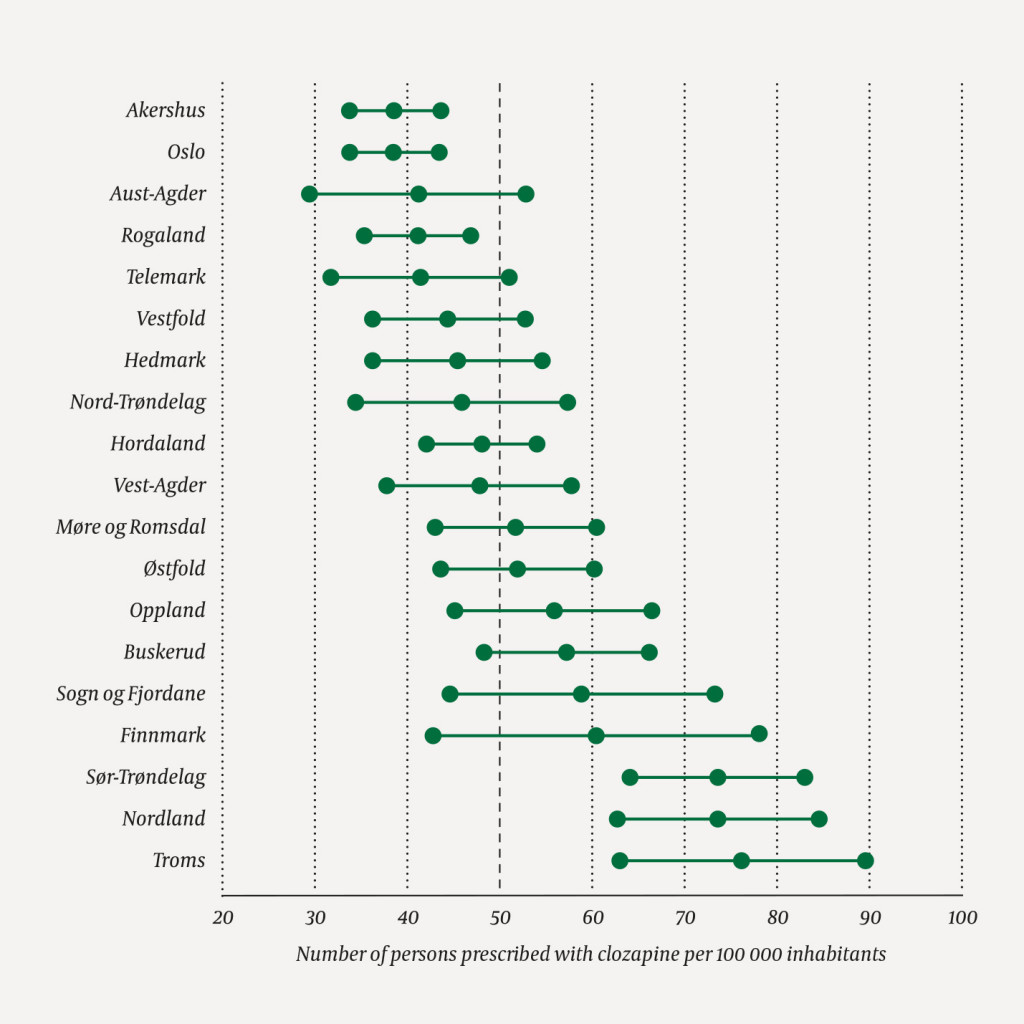
Table 1
Proportion of the population prescribed with clozapine in Norwegian counties in 2016.
| County | Number prescribed with clozapine | Total population | Proportion of the population that uses clozapine (%) |
|---|---|---|---|
| Akershus | 232 | 599 428 | 0.039 |
| Aust-Agder | 48 | 116 220 | 0.041 |
| Buskerud | 160 | 278 686 | 0.057 |
| Finnmark | 46 | 75 946 | 0.061 |
| Hedmark | 89 | 195 766 | 0.045 |
| Hordaland | 250 | 518 245 | 0.048 |
| Møre og Romsdal | 138 | 265 774 | 0.052 |
| Nordland | 179 | 242 408 | 0.074 |
| Nord-Trøndelag | 63 | 136 806 | 0.046 |
| Oppland | 106 | 189 214 | 0.056 |
| Oslo | 258 | 662 511 | 0.039 |
| Rogaland | 195 | 471 062 | 0.041 |
| Sogn og Fjordane | 65 | 109 904 | 0.059 |
| Sør-Trøndelag | 232 | 315 336 | 0.074 |
| Telemark | 72 | 172 908 | 0.042 |
| Troms | 126 | 164 974 | 0.076 |
| Vest-Agder | 88 | 183 409 | 0.048 |
| Vestfold | 110 | 246 698 | 0.045 |
| Østfold | 152 | 291 330 | 0.052 |
| Total | 2 609 | 5 236 625 | 0.050 |
Proportion of patients and prescribing rate
The proportion of patients followed up by the specialist health services for the diagnosis of schizophrenia varied between the counties (0.13 %–0.27 %). There was no significant correlation between the proportion of patients followed up by the specialist health services for the diagnosis of schizophrenia on the one hand, and the prescribing rate for clozapine on the other (Spearman's correlation coefficient 0.17, p = 0.50). The county of Oslo stood out in having a low prescribing rate for clozapine in relation to the proportion of patients with schizophrenia. Nor was there any significant correlation when Oslo was excluded from the analyses (Spearman's correlation coefficient 0.36, p = 0.15).
Prescribing rates in regional health authorities
Figures 2a and 2b show the prescribing rates for clozapine in 2016 in the regional health authorities by sex and age group. Clozapine was prescribed 1.6 times more frequently in the region with the highest prescribing rate (Northern Norway Regional Health Authority, 73 (95 % CI 65–80) per 100 000 inhabitants) when compared to the region with the lowest prescribing rate (South-Eastern Norway Regional Health Authority, 45 (95 % CI 42–47) per 100 000 inhabitants).
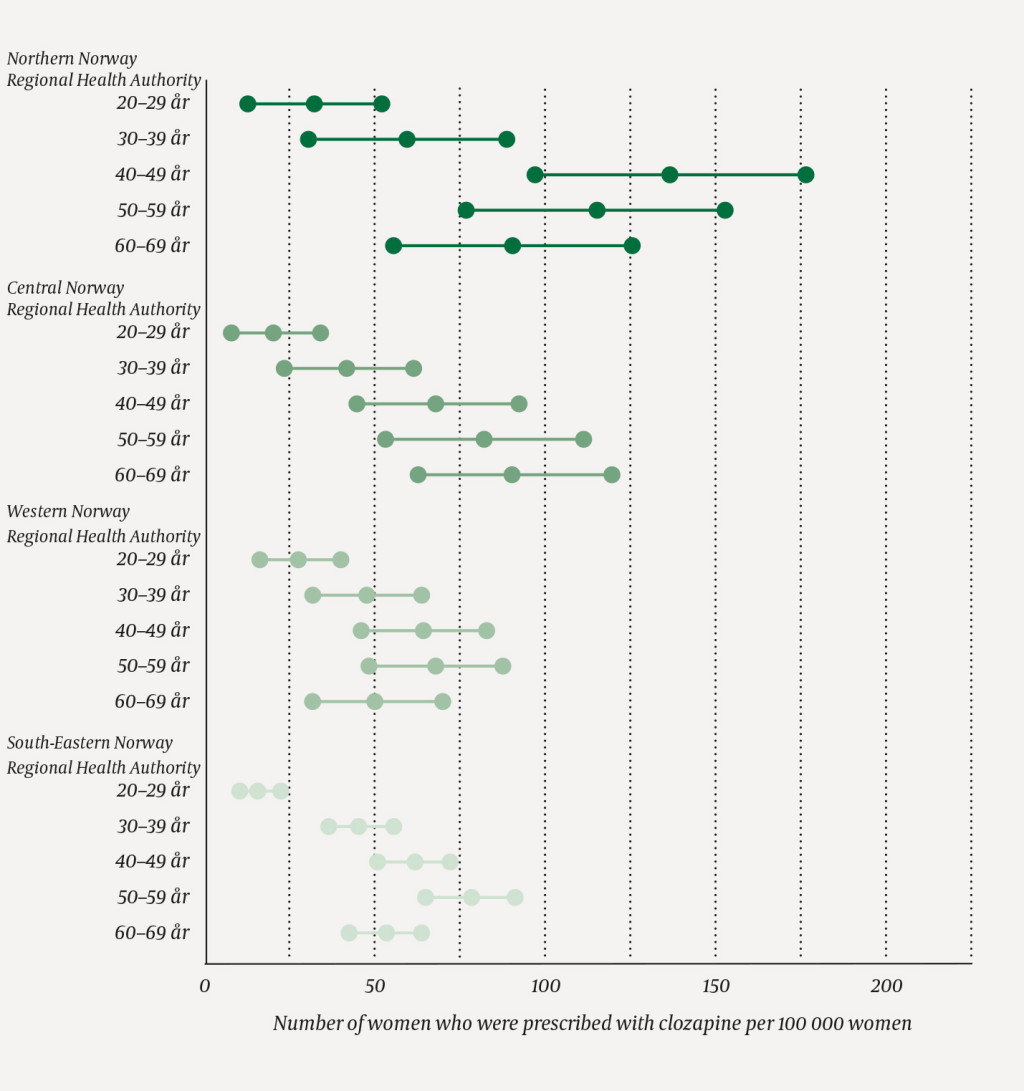
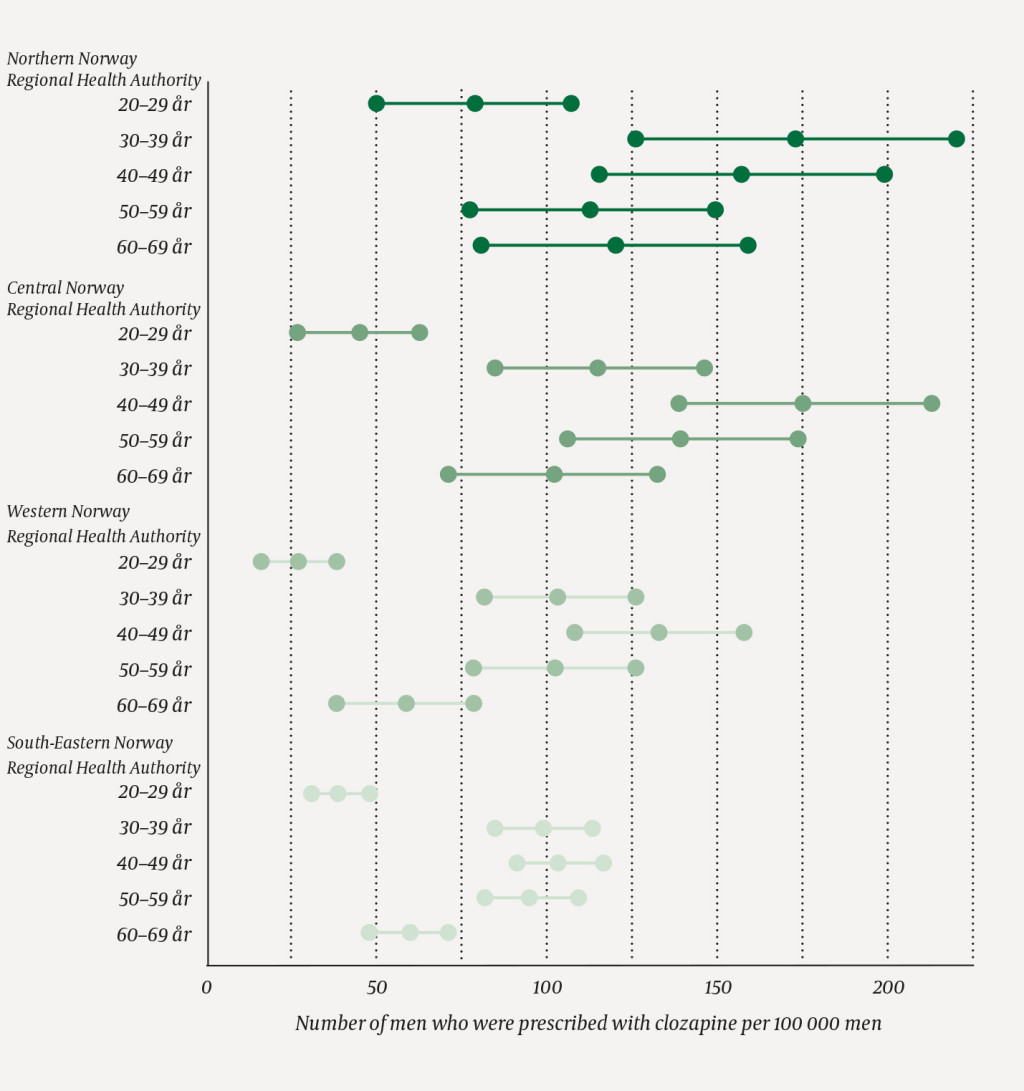
The greatest difference in the prescribing rate was observed among men in the age group 20–29 years, where clozapine was prescribed 2.9 times more frequently in the region with the highest prescribing rate when compared to the region with the lowest prescribing rate. In Northern Norway Regional Health Authority, the highest prescribing rate was among women in the age group 40–49 years, whereas in the other regional health enterprises the peak in the prescribing rate came later (50–59 years and 60–69 years). Among men, the prescribing rate peaked ten years earlier in Northern Norway Regional Health Authority (30–39 years) than in the other health authorities (40–49 years).
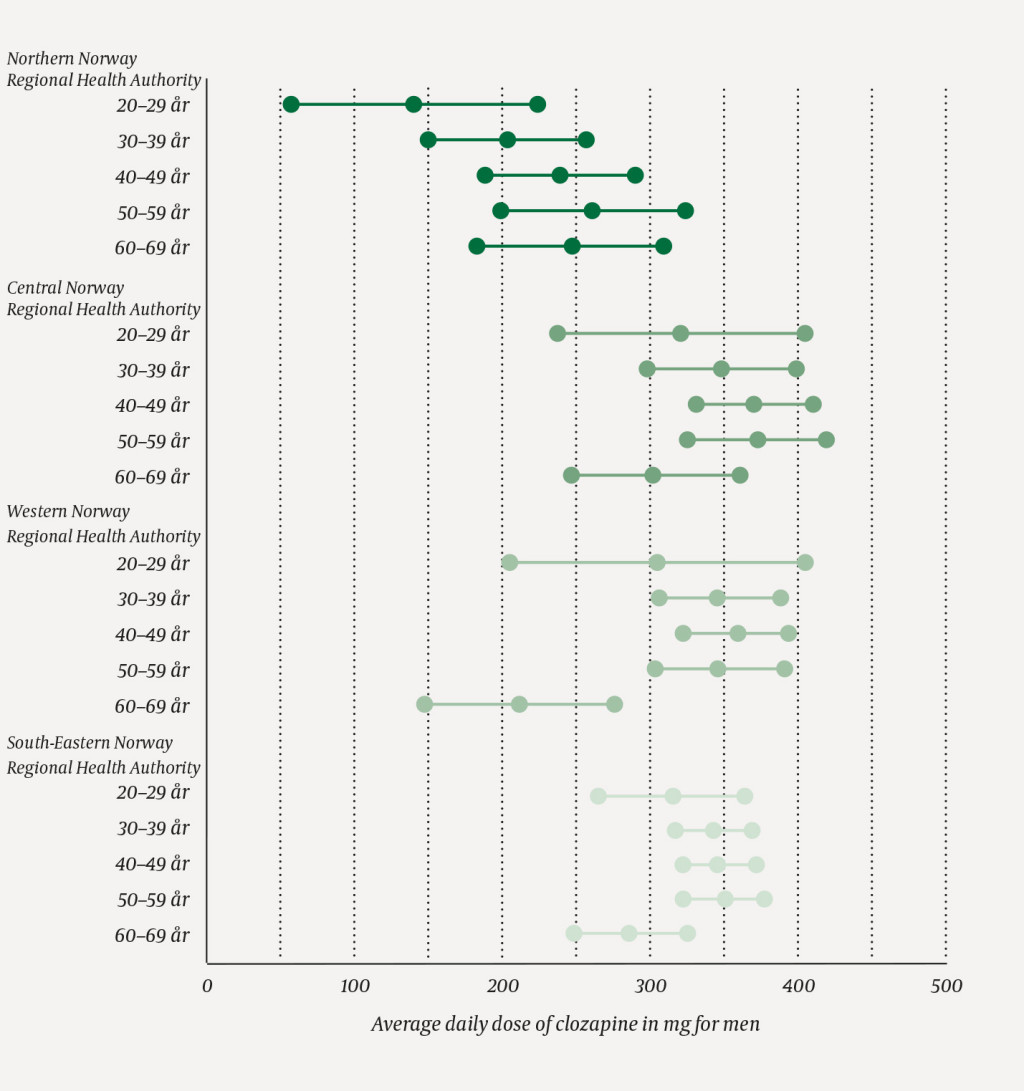
The average prescribed dose of clozapine for women and men in different age groups in 2016 is shown in Figures 3a and 3b. The age group 20–24 years is not included because of missing data from the Norwegian Prescription Database. Clozapine was prescribed in doses that were 1.4 times higher in the region with the highest average dose (Central Norway Regional Health Authority, 331 mg (95 % CI 313–349)) when compared to the region with the lowest prescribed average dose (Northern Norway Regional Health Authority, 235 mg (95 % CI 215–255)). Northern Norway Regional Health Authority had the lowest prescribed average dose in all age categories for both women and men, with the exception of the age group 60–69 years.

The prescribing rates per 100 000 inhabitants for antipsychotic drugs as a group were for Northern Norway Regional Health Authority 1 746 (95 % CI 1 709–1 783), Central Norway Regional Health Authority 1 814 (95 % CI 1 783–1 845), Western Norway Regional Health Authority 1 959 (95 % CI 1 933–1 985) and South-Eastern Norway Regional Health Authority 2 319 (95 % CI 2 302–2 336). Clozapine accounted for a small proportion of the prescribing of antipsychotic drugs as a group: 4.2 % in Northern Norway Regional Health Authority; 3.3 % in Central Norway Regional Health Authority; 2.4 % in Western Norway Regional Health Authority: and 1.9 % in South-Eastern Norway Regional Health Authority.
Discussion
This study describes geographical variations in prescribing practices for clozapine in Norway in terms of the prescribing rate, average doses and the sexes and age groups for which this drug is most frequently used.
Differences between Norwegian counties
In 2016, clozapine was prescribed nearly twice as frequently in Nordland, Sør-Trøndelag and Troms counties as in Oslo and Akershus county. A possible explanation for these differences could be variations in prevalence of the diagnosis of schizophrenia. Having reviewed data from the Norwegian Patient Registry, however, we cannot find any significant correlation between the prescribing rates for clozapine and the proportion of the population followed up by the specialist health services for the diagnosis of schizophrenia. A number of previous studies have shown an elevated risk of schizophrenia among people resident in urban areas, when compared to rural areas (7, 17). We nevertheless find that the Oslo county stands out in having a low prescribing rate for clozapine. Possible explanations could be that the average patient with schizophrenia in Oslo has a better treatment response to other antipsychotic drugs or has less severe symptoms, and thus is not prescribed with clozapine.
The topic of geographical variations in treatment response has been little explored. In a Danish registry study, the authors found that the prevalence of treatment resistance was lower in urban areas (18), but it is unclear whether this is a matter of genuine differences in illness, or whether other factors, such as treatment practices, play a role. Whether patients with schizophrenia in Oslo have a higher prevalence of co-morbid addiction disorders when compared to other Norwegian regions is also a matter for speculation. An unstable lifestyle with little opportunity for follow-up with regular blood sampling might be a reason to preclude the choice of this drug. Finally, relative underuse, in the sense that the drug is used more rarely in Oslo than in other counties even though all patient-related characteristics are identical, may explain our findings.
Differences between regional health authorities
Northern Norway Regional Health Authority differed from the other regional health authorities in several respects. They had by far the highest prescribing rate for clozapine, and prescribed it more frequently to younger patients and in smaller average doses when compared to the other regional health authorities. These figures are in apparent contradiction to the observation that Northern Norway Regional Health Authority has the lowest prescribing rate for antipsychotic drugs as a group.
One possible interpretation of these figures is that Northern Norway Regional Health Authority more frequently initiates the recommended drug-based therapy for treatment-resistant schizophrenia (clozapine) at an earlier stage and thus needs smaller doses, and secondary to this has a lower total use of antipsychotic drugs. It is important to emphasise, however, that no conclusions regarding treatment quality can be drawn on the basis of observational registry studies such as this one. Other possible explanations for the low average doses in Northern Norway Regional Health Authority could be that combination therapies involving multiple antipsychotic drugs are used more frequently, or that clozapine is used for other indications (for example Parkinson's disease, for which considerably smaller doses are recommended (19)). The low total prescribing rate of antipsychotic drugs as a group and the relatively low prescribing rate and large average dose of clozapine to the oldest patient groups in Northern Norway Regional Health Authority run counter to these explanations.
Figures from the regional health authorities show that the prescribing of clozapine reaches its peak later for women than for men. This could possibly be explained by the later debut of schizophrenia among women compared to men (20). Furthermore, the figures show that women are prescribed with clozapine more rarely than men. One explanation for this could be that schizophrenia in general (8), and possibly also treatment resistance (20), occur more rarely in women than in men. Determining whether these sex differences reflect a practice of prescribing clozapine more rarely to women, even when an indication of treatment-resistant schizophrenia has been established, will be an important topic for further research.
Geographical differences in the prescribing of clozapine have also been described in other countries (9, 21). The authors of these articles point to local variations in treatment practices as a key cause. Variations in psychiatrists' attitude to and knowledge about clozapine are likely to be an important element of this explanation (22). In light of the fact that clozapine is prescribed more rarely (9, 10, 21) and later (12) in the course of illness than what is recommended, one interpretation of the geographical differences shown in this study is that a proportion of the patients with treatment-resistant schizophrenia are not provided with optimal drug-based therapy.
Future research should seek to clarify the extent to which clinicians possess sufficient knowledge about clozapine to make this drug a real alternative for patients with treatment-resistant schizophrenia. A more consistent practice can be achieved by increasing the focus on identification of and interventions against treatment-resistant schizophrenia in the training of mental healthcare personnel.
Strengths and weaknesses
The strength of this study is that the analyses have been undertaken on complete national data on clozapine dispensed from pharmacies. This comprehensive material has enabled comparisons not only between regions, but also between sexes and age groups. It is a weakness that prescribing in hospitals, where treatment with clozapine tends to be initiated (21), is not included in the data. We cannot exclude the possibility that clozapine is more often tried out in outpatient settings in counties where patients need to travel long distances. If so, the data from the Norwegian Prescription Database will overestimate the relative prescribing in counties where the hospitals are far apart. Moreover, our data reveal no information regarding the indications for prescribing clozapine, combination therapy with other antipsychotic drugs or whether the drug has been used as prescribed. Another key point is that clozapine is also used for other chronic psychoses such as delusional disorder (F22.0) and schizoaffective disorder (F25.0), as well as psychosis associated with Parkinson's disease. We chose to retrieve data for the proportion of patients with the diagnosis of schizophrenia in different regions and did not include the other diagnostic groups.
Conclusion
The Norwegian national guidelines recommend clozapine to patients with schizophrenia after two failed treatment attempts with other antipsychotic drugs. In this study we found differences by county in the prescribing of clozapine that cannot be explained by variations in the proportion of the population that receives treatment for the diagnosis of schizophrenia. Patients with treatment-resistant schizophrenia tend to have serious illness trajectories, and local guidelines need to ensure that the patients are offered the recommended drug-based treatment.
We wish to thank Arne E. Vaaler for his comments to a draft of the article.
The article has been peer reviewed.
- 1.
Leucht S, Cipriani A, Spineli L et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 2013; 382: 951–62. [PubMed][CrossRef]
- 2.
Helsedirektoratet. Nasjonal faglig retningslinje for utredning, behandling og oppfølging av personer med psykoselidelser. https://www.helsedirektoratet.no/tema/psykose Lest 18.6.2019.
- 3.
National Institute for Health and Care Excellence (NICE). NICE guidline. Psychosis and schizophrenia in adults: prevention and management. Clinical Guideline cg178. https://www.nice.org.uk/Guidance/CG178 Lest 18.6.2019.
- 4.
Kane J, Kishimoto T, Correl CU. Evaluation and management of treatment-resistant schizophrenia UpToDate versjon 11.0, 2018. https://www.uptodate.com/contents/evaluation-and-management-of-treatment-resistant-schizophrenia Lest 18.6.2019.
- 5.
BMJ Best Practice. Schizophrenia, Treament algorithm. https://bestpractice.bmj.com/topics/en-gb/406/treatment-algorithm Lest 18.6.2019.
- 6.
Bachmann CJ, Aagaard L, Bernardo M et al. International trends in clozapine use: a study in 17 countries. Acta Psychiatr Scand 2017; 136: 37–51. [PubMed][CrossRef]
- 7.
Castillejos MC, Martín-Pérez C, Moreno-Küstner B. A systematic review and meta-analysis of the incidence of psychotic disorders: the distribution of rates and the influence of gender, urbanicity, immigration and socio-economic level. Psychol Med 2018; 48: 1–15. [PubMed][CrossRef]
- 8.
McGrath J, Saha S, Chant D et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev 2008; 30: 67–76. [PubMed][CrossRef]
- 9.
Stroup TS, Gerhard T, Crystal S et al. Geographic and clinical variation in clozapine use in the United States. Psychiatr Serv 2014; 65: 186–92. [PubMed][CrossRef]
- 10.
Gotfredsen DR, Wils RS, Hjorthøj C et al. Stability and development of psychotic symptoms and the use of antipsychotic medication - long-term follow-up. Psychol Med 2017; 47: 2118–29. [PubMed][CrossRef]
- 11.
Kroken RA, Johnsen E, Ruud T et al. Treatment of schizophrenia with antipsychotics in Norwegian emergency wards, a cross-sectional national study. BMC Psychiatry 2009; 9: 24. [PubMed][CrossRef]
- 12.
Howes OD, Vergunst F, Gee S et al. Adherence to treatment guidelines in clinical practice: study of antipsychotic treatment prior to clozapine initiation. Br J Psychiatry 2012; 201: 481–5. [PubMed][CrossRef]
- 13.
Pakkeforløp for utredning og behandling i psykisk helsevern, voksne (gjelder fra 1. januar 2019). IS-2641. Oslo: Helsedirektoratet, 2018. https://helsedirektoratet.no/retningslinjer/psykikse-lidelser-pakkeforlop-voksne Lest 18.6.2019.
- 14.
Folkehelseinstituttet. Reseptregistret. https://www.fhi.no/hn/helseregistre-og-registre/reseptregisteret/ Lest 18.6.2019.
- 15.
World Health Organization. WHO Collaborating Centre for Drug Statistics Methodology. https://www.who.int/medicines/regulation/medicines-safety/about/collab-centres-norwegian/en/ Lest 31.5.2018.
- 16.
Altman DG. Practical statistics for medical research. London: Chapman & Hall, 1991.
- 17.
Vassos E, Agerbo E, Mors O et al. Urban-rural differences in incidence rates of psychiatric disorders in Denmark. Br J Psychiatry 2016; 208: 435–40. [PubMed][CrossRef]
- 18.
Wimberley T, Pedersen CB, MacCabe JH et al. Inverse association between urbanicity and treatment resistance in schizophrenia. Schizophr Res 2016; 174: 150–5. [PubMed][CrossRef]
- 19.
Wilby KJ, Johnson EG, Johnson HE et al. Evidence-based review of pharmacotherapy used for Parkinson's disease psychosis. Ann Pharmacother 2017; 51: 682–95. [PubMed][CrossRef]
- 20.
Abel KM, Drake R, Goldstein JM. Sex differences in schizophrenia. Int Rev Psychiatry 2010; 22: 417–28. [PubMed][CrossRef]
- 21.
Nielsen J, Røge R, Schjerning O et al. Geographical and temporal variations in clozapine prescription for schizophrenia. Eur Neuropsychopharmacol 2012; 22: 818–24. [PubMed][CrossRef]
- 22.
Nielsen J, Dahm M, Lublin H et al. Psychiatrists' attitude towards and knowledge of clozapine treatment. J Psychopharmacol 2010; 24: 965–71. [PubMed][CrossRef]