Sick leave is a topical subject in the context of the 2010 revision of the Agreement on a More Inclusive Working Life (the IA agreement) (1, 2). There has been little discussion about the extent to which sick leave may be related to work, although this may be highly important with respect to what measures will be effective in reducing sick leave and expulsion from work. So far, the IA agreement has primarily focused on reducing the level of sick leave through measures designed to help the sick return to work (secondary prevention) rather than on measures designed to prevent people from being sick-listed in the first place (primary prevention) (3). The proposals tabled by the group of experts appointed by the Norwegian Ministry of Labour to assess possible administrative initiatives to reduce sick leave included hardly any primary preventive measures (4).
This paper provides an overview of the extent to which sick leave may be work-related, i.e. be linked to work or workplace conditions.
Material and methods
The paper is based on a non-systematic literature search using PubMed and a discretionary selection of articles based on personal knowledge of the field and experience gained through my own studies.
What does «work-related» mean?
All sick leave may be said to be work-related in the sense that the employee finds it difficult to carry out his/her job due to illness, i.e. «health-related work problems». However, this definition is not particularly useful in terms of workplace prevention. «Work-related health problems» are often defined as health problems (illness or injury) which are partly or entirely caused or aggravated by working conditions (5) – (7). Workplace intervention may prevent or reduce such health problems as well as the resulting sick leave.
Is there a causal link between work and ill health?
The relationship between certain working conditions and ill health is well documented. As early as in 1700 Italian physician Ramazzini listed diseases associated with more than 50 occupations (8). In Finland, it is estimated that 7 per cent of all fatalities in the relevant disease and age categories may be attributed to occupational factors, a higher proportion among men (10 per cent) than among women (2 per cent), and a total of 4 per cent of all fatalities, irrespective of age and diagnosis (9). It is estimated that approximately 20 per cent of lung cancers among Norwegian men would have been avoided were it not for occupational exposure (10, 11). The same applies for 85 per cent of all malignant mesotheliomas, a type of cancer which is most often caused by asbestos exposure at work, and 32 per cent of nasal and sinus cancers (10). Based on epidemiological literature, the American Thoracic Society estimates that approximately 15 per cent of asthma instances among adults, and 15 per cent of COPD (chronic obstructive pulmonary disease) in the general population, may be attributed to work (12).
Work-related health problems are very common. Approximately 60 per cent of respondents in the Oslo Health Study (the HUBRO study) reported that they had suffered from health problems caused by working conditions in the course of the last month (13). Neck/shoulder pain and low back pain were the most common; these were attributed to working conditions by respectively 3/4 and 1/2 of the respondents with such pain. The data included health problems of all severities and it is probable that people with light symptoms rarely take sick leave. Statistics Norway’s Level of living survey 2006 showed that among the economically active with work-related musculoskeletal disorders, approx. 15 per cent reported to suffer «great pain» and 25 per cent «some pain»; the corresponding figures for respondents with mental symptoms were 7 per cent and 20 per cent respectively.
Work-related health problems also constitute a frequent motivation for people to seek a doctor. A study conducted by Hilt et al. among economically active patients attended to by a GP, found that 40 per cent of women and 54 per cent of men considered their health problem to be possibly or definitely caused by work (14). Two Nordic studies based on GP assessments showed that one in five consultations was probably or possibly work-related; for musculoskeletal disorders the proportion was even higher (between 1/3 and 1/2) (15, 16). The GP assessments may have been too low. In 2006 only 7 per cent of Norwegian GPs reported work-related diseases to the Norwegian Labour Inspection Authority (17), which may indicate that many medical practitioners are little aware of the work-relatedness of diseases.
Is there a causal link between sick leave and work?
Figure 1 is a simple model showing the relationship between work and sick leave. Working conditions may have an impact, whether through negative health effects or through the demands of the work. The need to take sick leave will depend on the interaction between the individual’s health and job demands (18). Consequently, the same illness or impairment may result in different rates of incapacity to work due to dissimilar job demands (19).
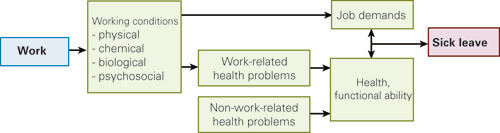
Work may also influence sick leave through psychological and social mechanisms, which may impact on factors such as motivation. These are not included in this simple model and will not be further discussed in this paper; they would however be important factors in a more comprehensive biopsychosocial model (20). Also, individual factors such as age, gender and personality have an impact.
Self-reported work-related illness
In the Level of living survey 2006, 18 per cent of all economically active respondents reported that they had taken at least one sick leave of more than 14 days’ duration in the course of the last 12 months. Approximately 40 per cent of them answered that their absence was due to health problems which partly or entirely was caused by their job (21). This constitutes 7 per cent of the working population, somewhat higher among women (8 per cent) than among men (5 per cent). A similar figure (7 per cent of the working population) was found in a later survey of work-related illnesses and injuries in connection with Statistics Norway’s Labour force survey 2007, involving slightly different questions (22). The data showed great variation with occupation, ranging from less than 1 per cent in the group of doctors, dentists, pharmacists and veterinary surgeons to 13 per cent among cleaners, food workers, cooks and catering assistants. The proportion of sick leaves that were reported to be work-related varied significantly as well, from 5 per cent to 50 per cent for the above-mentioned occupations (21).
Tellnes et al. conducted a study of sick leave among 118 GPs and their patients in the Buskerud area and found that heavy physical work was assessed by the doctor and/or patient to be a contributing cause of the illness leading to sick leave in 48 per cent of patients (23). The work-related proportion was considerably higher among patients with musculoskeletal disorders (78 per cent), particularly if they were involved with heavy physical work or were standing or walking a great deal at work (in excess of 90 per cent). Psychological factors associated with work were considered to be a contributing cause of illness for 32 per cent of absentees. There were great variations depending on the type of health problem and the type of work.
Can we trust self-reporting?
Questionnaires are often used to investigate work-related health problems; this is the case for Statistics Norway’s Level of living surveys as well as the European Working Conditions Surveys (24). Many have a sceptical attitude to this kind of self-reporting and hold the opinion that the individuals themselves will tend to over-estimate the correlation with work. The HUBRO study compared self-reporting to physician assessment for 217 people suffering from neck/shoulder or arm pain (25). The doctors used criteria drawn up by a group of European experts to assess whether the pain might be caused by working conditions (26). The sufferers themselves considered their pain to be work-related slightly more often than the physicians: 80 per cent versus 65 per cent for neck/shoulder pain, and 78 per cent versus 72 per cent for arm pain. Consequently, self-reporting appears to give a reasonably good measure of the work-related proportion of health problems, but this may vary with the type of health problem and the criteria for assessing the work-relatedness (25).
Work-related illness and work capacity
There is much evidence that people with work-related health problems have more sick leaves than people with similar health problems caused by factors other than their work. Individuals who are taken ill for reasons associated with their work will evidently have a greater need for absence from the work that made them ill. Leira et al. surveyed people who had been on sick leave for more than 16 days due to asthma and found that as much as 70 per cent had work-related asthma, based on reports of respiratory symptoms suffered at work and improving symptoms when absent from work (27). This is significantly higher than in the general population, as demonstrated, for instance, by the HUBRO study which showed that 18 per cent of people with asthma symptoms attributed their symptoms to work (13). A Finnish study showed that the risk of full incapacity to work was nearly 13 times higher among patients who reported work-related health problems than among those who reported non-work-related health problems (28).
The significance of work environment factors
A number of work-related factors have been studied in relation to sick leave, particularly physical/ergonomic factors such as heavy physical work, awkward work postures and repetitive work, psychosocial working conditions such as psychological job demands, job control and social support in the workplace, and organisational factors such as shift work. A comprehensive study of the causes of sick leave carried out in 2004 (29) found limited scientific evidence that physical working conditions – particularly heavy physical work – have an effect on sick leave, and moderate evidence of a causal connection with low job control (30). However, among people who were sick-listed due to back disorders, it was found that a number of factors had an effect, among them low job satisfaction (moderate documentation), low job control, and work involving heavy lifting or a bent/twisted working position (limited documentation) (31). Despite a great number of studies and well documented statistical associations between working conditions and sick leave, it was nevertheless concluded that the scientific documentation to support a causal relationship was generally limited, especially due to problems with selection or confounding (30). Even if the association between disease and certain working conditions is well documented, most people who suffer from a disease are not on sick leave, a fact which may contribute to the relatively weak documentation (32).
In Denmark a number of longitudinal studies have been conducted in which attempts have been made to reduce the weaknesses of earlier research (33). These studies have combined the use of data from questionnaires and records, and they have studied factors that impact on different stages of the sick leave process (34).
They estimated that the number of people taking more than six sick days per year could have been 40 per cent lower if everyone’s physical and psychosocial work environment had matched the standard of that enjoyed by the 10 per cent with lowest exposures (35). Other studies from Denmark have shown similar figures (36). Heavy physical work such as heavy lifting/carrying or pushing/pulling, and awkward work postures such as standing up/squatting or a bent /twisted neck/back, appear to be particularly important (37). Many psychosocial job factors appear to be important, such as job control (work autonomy), social support from supervisors, psychological job demands, predictability and role conflicts (33, 38). The results vary somewhat from study to study and between women and men, particularly with respect to psychosocial factors (33). The attributable proportion of sick leave was found to be higher for work-related factors than for life style factors such as smoking (26 per cent among women and 17 per cent among men) (39).
Social inequalities in health are well documented and working conditions have been shown to influence these differences (40). A Danish study found that physical and psychosocial working conditions could explain as much as 40 – 50 per cent of long-term sick leave differences between the highest and the lowest social classes (managers/academics and skilled/unskilled workers respectively), adjusted for life style and other factors (41).
The significance of structural working conditions
Many studies have shown that structural conditions, such as re-organisation and workforce downsizing, can bring higher rates of sick leave, disability retirement and mortality in the following years (42) – (46). This is the case for people who are directly affected (42, 43) but also for people who remain in the company after it has been downsized (43, 46). Tougher job demands, lower job control and higher job insecurity in connection with the downsizing are all factors shown to have an impact on health and sick leave (47). A project entitled «The new state» found that the increase in sick leave in the Norwegian Postal Service and the Public Roads Administration/Mesta after the workforce was downsized in the mid 1990s, could largely be explained by longer periods of sick leave (44). However, other studies have indicated unaltered or lower rates of sick leave after downsizing operations (48, 49). This is interpreted as «sickness presenteeism», i.e. that people attend work even if they are ill, particularly people in time restricted employment or with lower job security (46, 48).
Preventing sick leaves caused by work-related illness
Incapacity to work is a relational concept and must be seen in the context of the individual’s resources and the demands he/she encounters at work (18). If there is a mismatch between an individual’s level of functional ability and his/her job demands, this may give rise to problems in carrying out the work and therefore a need for sick leave (50). This type of imbalance may be caused by illness and impaired health while job demands remain unaltered, or by increasing job demands while health and functional ability remain the same, for example in connection with a re-structuring process or workforce downsizing (18). There will often be a combination of the two varieties.
Workplace interventions to prevent work-related illness may also prevent sick leave. Furthermore, such workplace initiatives may often make it possible to prevent or shorten sick leave periods caused by an imbalance between individual resources and job demands, irrespective of the primary cause of the imbalance. This will apply to most cases of sick leave, which therefore must be considered work-related in a wider sense. This will include «job related functional absence», but also to a great extent «relative functional absence» as per Bruusgaard & Claussen’s categorisation of sick leave (51).
At the moment there is relatively limited documentation available concerning the effect of workplace intervention on sick leave. A recently published Cochrane review based on six randomised controlled trials concluded that there is moderate-quality evidence to support the use of workplace interventions to reduce sick leave among workers with musculoskeletal disorders when compared to usual care (52). More recent randomised intervention studies have shown that the screening of employees by an occupational health assessment followed by intervention vis-a-vis people with a higher risk of long-term sick leave, may produce a 30 – 40 per cent reduction in the number of sick days (53) – (55).
Workplace interventions aimed at pregnant women have been shown to reduce sick leave during pregnancy. A project carried out in the South Troms area demonstrated a reduction in the average length of sick leaves from approx. 16 to 2.4 weeks (85 per cent), while the use of graded sick leave increased (56). A study based on the Norwegian Mother and Child Cohort Study confirms the importance of making job adjustments to accommodate pregnant women. Kristensen et al. found that half the pregnant women who experienced a need for job adjustments but who had never benefited from such, took more than two weeks of sick leave between week nos. 17 and 30 of the pregnancy, whereas women who had benefited from such arrangements had an 11 per cent lower risk (57).
Discussion
This literature review shows that sick leave is often work-related, either in a narrow sense, when the absence from work is caused by work-related illness or injury, or in a wider sense, when the absence is caused by an imbalance between individual resources and job demands. In both cases workplace interventions may prevent or shorten the period of sick leave.
Many resources are expended on initiatives designed to help the sick return to work, by doctors, employers and the Norwegian Labour and Welfare Administration (NAV). However, more importance should be attached to primary preventive measures designed to reduce work-related illness and workplace interventions designed to accommodate people who carry a higher risk of absence, before they get sick-listed. For many, it will take a long time before they are capable of resuming work.
Employers have an obvious responsibility, but often fail to see the need to take action before the employee falls seriously ill or has taken sick leave. Medical practitioners may see the need, but are often insufficiently briefed on work-related matters and have no contact with employers. The occupational health service possesses knowledge about the relationship between work and health and also has a route of contact with the employer. The occupational health service should play a central part in this context, but its role remains obscure within the current IA agreement. The service is probably underused by everyone ranging from the treating physicians to the employers, the employees and the Norwegian Labour and Welfare Administration.
The IA agreement has three objectives, but so far most of the focus has been on reducing sick leave. Measures that help us succeed in including the elderly and those with reduced work capacity will enable these people to remain in employment, albeit with a somewhat higher rate of absence. This may however be a low price to pay for keeping as many as possible in employment?
I would like to thank Helge Kjuus at the National Institute of Occupational Health for providing his comments on my manuscript.
Conflicting interests listed:
None
Tabell
| Main points |
|
- 1.
Intensjonsavtale om et mer inkluderende arbeidsliv. Oslo: Arbeids- og administrasjonsdepartementet, 2001.
- 2.
Intensjonsavtale om et mer inkluderende arbeidsliv 1. mars 2010 – 31. desember 2013 (IA-avtalen). Oslo: Arbeidsdepartementet, 2010.
- 3.
Ose SO, Bjerkan AM, Pettersen I et al. Evaluering av IA-avtalen (2001–2009). SINTEF-rapport nr. A11947. Trondheim: SINTEF Teknologi og samfunn, 2009.
- 4.
Tiltak for reduksjon i sykefravær: Aktiviserings- og nærværsreform. Ekspertgrupperapport. Oslo: Arbeidsdepartementet, 2010.
- 5.
Verdens helseorganisasjon. Identification and control of work-related diseases. Rapport nr. 714. Genève: World Health Organization, 1985.
- 6.
Regulation (EC) No 1338/2008 of the European Parliament and of the Council of 16 December 2008 on Community statistics on public health and health and safety at work. http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2008:354:0070:01:EN:HTML (25.11.2010).
- 7.
Regulations (Standards – 29 CFR). Recording and reporting occupational injuries and illnesses. Determination of work-relatedness. Part Number 1904.5. Washington, DC: Occupational Safety & Health Administrations, 1972.
- 8.
Ramazzini B. Diseases of Workers. Translated from the Latin text De Morbis Artificum of 1713 by Wilmer Cave Wright. New York, NY: Hafner Publishing Company, 1964.
- 9.
Nurminen M, Karjalainen A. Epidemiologic estimate of the proportion of fatalities related to occupational factors in Finland. Scand J Work Environ Health 2001; 27: 161 – 213. [PubMed]
- 10.
Dreyer L, Andersen A, Pukkala E. Avoidable cancers in the Nordic countries. Occupation. APMIS Suppl 1997; 76: 68 – 79. [PubMed]
- 11.
Haldorsen T, Andersen A, Boffetta P. Smoking-adjusted incidence of lung cancer by occupation among Norwegian men. Cancer Causes Control 2004; 15: 139 – 47. [PubMed]
- 14.
Hilt B, Kvenild K, Stenersen H. Arbeidsrelaterte sykdommer i allmennpraksis. Tidsskr Nor Lægeforen 2003; 123: 2065–7. [PubMed]
- 15.
Kibsgård KA, Andersen JH, Rasmussen K. Arbejdsmedicin i almen praksis. En undersøgelse af arbejdsskaders omfang og art i Ringkjøbing Amt. Ugeskr Læger 1998; 160: 4863–7. [PubMed]
- 16.
Järhult B, Brühl P. Arbete som orsak till sjukdom. Läkartidningen 1986; 83: 3497 – 501. [PubMed]
- 17.
Samant Y, Parker D, Wergeland E et al. The Norwegian Labour Inspectorate’s Registry for Work-Related Diseases: data from 2006. Int J Occup Environ Health 2008; 14: 272 – 9. [PubMed]
- 18.
Westin S. Ervervsmessig uførhet – et forhold mellom individets ressurser og arbeidslivets krav. I: Bruusgaard D, Hatland A, Syse A, red. Et nødvendig gode. Folketrygdens plass i velferdssamfunnet. Oslo: AdNotam Gyldendal, 1994: 133–46.
- 20.
Knardahl S. Sykefravær har årsaker i individet, i virksomheten og i samfunnet. Oslo: Statens arbeidsmiljøinstitutt, 2010. www.stami.no/?nid=61605&lcid=1044 (28.10.2010).
- 21.
Tynes T, Eiken T, Grimsrud TK et al. Arbeidsmiljø og helse – slik norske yrkesaktive opplever det. Resultater fra Statistisk sentralbyrås levekårsundersøkelse for 2006. STAMI-rapport nr. 16/2008. Oslo: Statens arbeidsmiljøinstitutt, 2008.
- 22.
Gravseth HM. Arbeidsskader og arbeidsrelaterte helseproblemer. STAMI-rapport nr. 4/2010. Oslo: Statens arbeidsmiljøinstitutt, 2010.
- 24.
Parent-Thirion A, Fernández Macías E, Hurley J et al. Fourth European Working Conditions Survey. Dublin: European Foundation for the Improvement of Living and Working Conditions, 2007.
- 25.
Mehlum IS, Veiersted KB, Wærsted M et al. Self-reported versus expert-assessed work-relatedness of pain in the neck, shoulder, and arm. Scand J Work Environ Health 2009; 35: 222 – 32. [PubMed]
- 26.
Sluiter JK, Rest KM, Frings-Dresen MH. Criteria document for evaluating the work-relatedness of upper-extremity musculoskeletal disorders. Scand J Work Environ Health 2001; 27 (Suppl 1): 1 – 102. [PubMed]
- 27.
Leira HL, Berg JA, Bratt U et al. Mye arbeidsrelatert sykdom blant astmatikere. Tidsskr Nor Lægeforen 2006; 126: 2367–9. [PubMed]
- 29.
Alexanderson K, Norlund A, red. Sickness absence – causes, consequences, and practices. A systematic literature review by the Swedish Council on Technology Assessment in Health Care. Scand J Public Health Suppl 2004; 63.
- 33.
Lund T, Labriola M. Sickness absence in Denmark – research, results and reflections. Scand J Work Environ Health 2009; 7: 5 – 14.
- 34.
Labriola M. Conceptual framework of sickness absence and return to work, focusing on both the individual and the contextual level. Work 2008; 30: 377 – 87. [PubMed]
- 36.
Jensen C, Lund T, Mossing R et al. Arbejdsmiljø og fravær. København: Arbejdsmiljøinstituttet, 2002.
- 40.
Mehlum IS, Kristensen P, Kjuus H et al. Are occupational factors important determinants of socioeconomic inequalities in musculoskeletal pain? Scand J Work Environ Health 2008; 34: 250 – 9. [PubMed]
- 43.
Fevang E, Røed K. Omstillinger og nedbemanninger blant pleiere – en belastning for folketrygden. Søkelys på arbeidsmarkedet 2005; 22: 233–42.
- 44.
Trygstad S, Lorentzen T, Løken E et al. Den nye staten. Omfang og effekter av omstillingene i staten 1990–2004. Fafo-rapport 530. Oslo: Fafo, 2006.
- 45.
Rege M, Telle K, Votruba M. The effect of plant downsizing on disability pension utilization. J Eur Econ Assoc 2009; 7: 754 – 85. [CrossRef]
- 50.
Lindén V. Absence from work and work capacity. Bergen: Rikstrygdeverket, Bergen trygdekontor, 1967.
- 51.
Bruusgaard D, Claussen B. Ulike typer sykefravær. Tidsskr Nor Legeforen 2010; 130: 1834-6. [PubMed]
- 52.
van Oostrom SH, Driessen MT, de Vet HC et al. Workplace interventions for preventing work disability. Cochrane Database Syst Rev 2009; nr.2: CD006955. doi: 10.1002/14651858.CD006955.pub2. [PubMed]
- 56.
Gravid og i arbeid. Et pilotprosjekt i regi av Sør-Troms HMS-tjeneste. Tromsø: Sør-Troms HMS-tjeneste, 2009.