Splenic injury is a rare but potentially serious complication of colonoscopy. This case report illustrates the clinical course of a patient who suffered a splenic rupture following a technically challenging colonoscopy.
A woman in her 70s was referred for an outpatient colonoscopy due to suspected colorectal cancer. During the procedure, a large, friable tumour was found in the transverse colon. A biopsy was taken of the tumour, but the procedure had to be terminated due to technical difficulties and severe pain experienced by the patient. She was admitted for observation and further evaluation of malignancy. Contrast-enhanced computed tomography (CT) of the thorax, abdomen and pelvis was performed in the portal venous phase on the same day. A stenosing tumour was found in the transverse colon, with no evidence of metastases. The patient had two episodes of blood in the stool following the colonoscopy but was otherwise well. The following day, she was discharged home in good health, and an elective laparoscopic extended right hemicolectomy was scheduled.
Three days later, the patient was readmitted due to the sudden onset of sharp, stabbing pains in the upper left abdomen and back. Prehospital treatment included 50 µg of fentanyl and 1 g of paracetamol administered intravenously, which provided effective relief. On clinical examination in the emergency department, the patient had a soft abdomen with normal bowel sounds on auscultation. She had localised tenderness in the upper left quadrant, and a faecal occult blood test was instantly positive. Vital signs were unremarkable. Blood tests showed a drop in haemoglobin following the colonoscopy, from 11.7 g/dL (reference range 11.7–15.3) to 10.6 g/dL upon arrival at the emergency department, as well as a low iron level of 4 µmol/L (reference range 9–34). The patient's pain subsided, and she was admitted for observation.
The following day, the patient again developed severe abdominal pain similar in nature to that at admission. However, she was now tender to palpation in the entire abdomen, with rebound tenderness in the upper left quadrant and around the navel. She exhibited symptoms of hypovolemic shock, with a blood pressure of 85/60 mmHg and a pulse of 100–105 beats per minute. Her haemoglobin level had further dropped to 8.5 g/dL. Consequently, the patient was given two units of erythrocytes (SAG) and two units of Octaplasma.
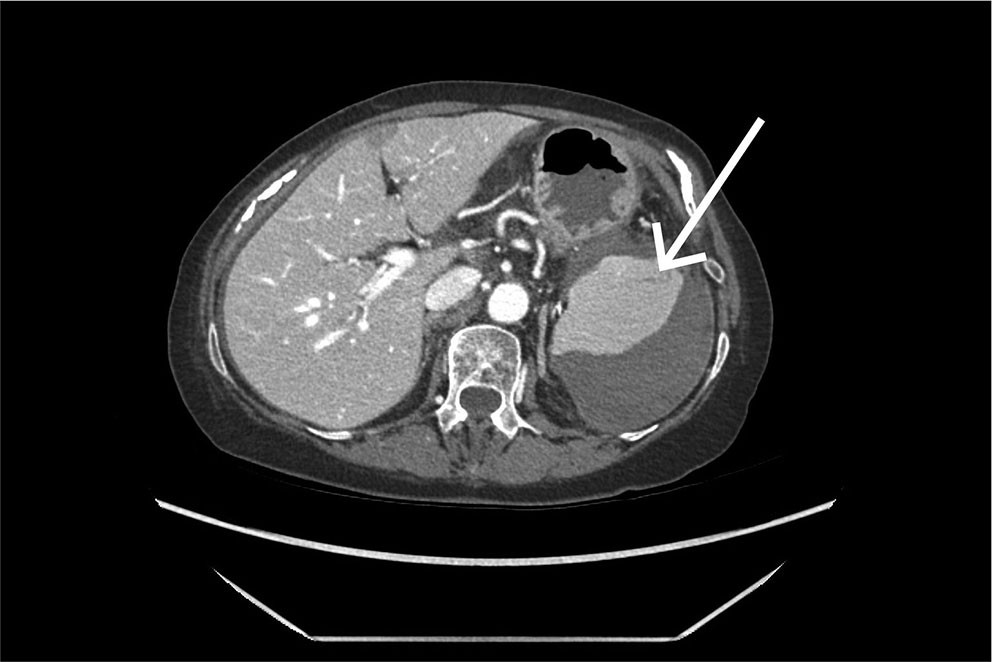
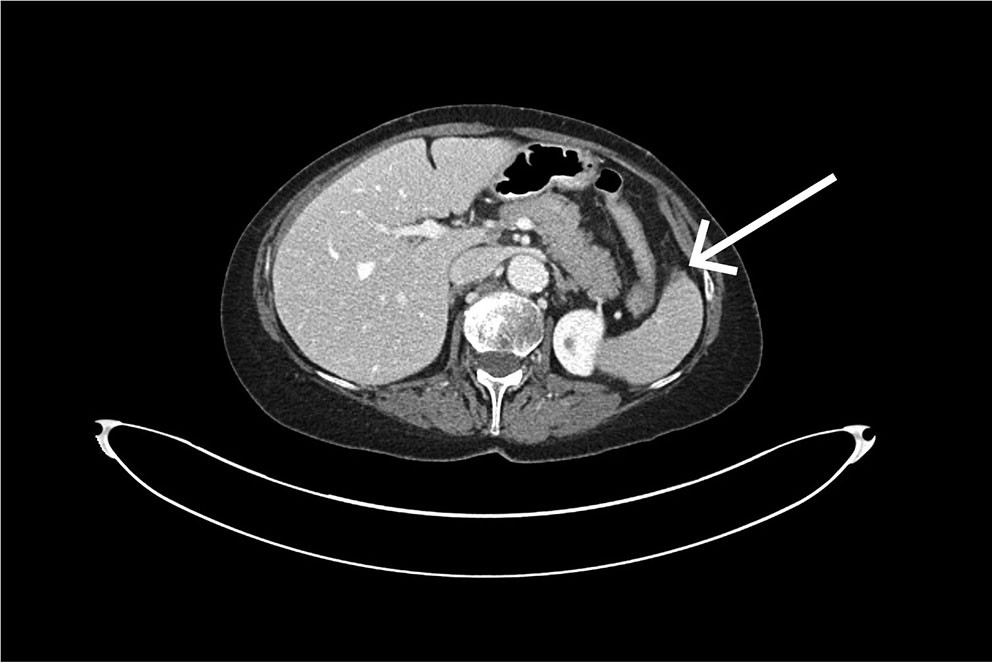
An urgent CT scan of the abdomen and pelvis with intravenous contrast in the portal venous phase was performed. The examination revealed a large subcapsular splenic haematoma and a small splenic laceration (Figure 1). It was concluded that a capsular rupture had likely occurred, with bleeding into the free abdominal cavity and fluid accumulation around the liver, colon and pelvis. Upon re-examination of the CT scan taken immediately after the colonoscopy, a small subcapsular splenic laceration was visible near the attachment of the splenocolic ligament (Figure 2).
Angiographic intervention was considered, but due to an ostial stenosis of the celiac trunk, the conditions were unsuitable for coiling of the splenic artery.
An emergency laparotomy with splenectomy and subtotal colectomy was planned due to the presence of a tumour in the colon. During surgery, fresh blood was observed in the abdomen and a large clot in the spleen, supporting the suspicion of a ruptured splenic haematoma.
The patient had an uncomplicated postoperative course and was discharged in good health 11 days after surgery.
Discussion
In blunt abdominal trauma, the spleen is the organ most often injured (1). In the context of colonoscopy, splenic injury is a rare but potentially serious complication (2).
The spleen is a richly vascularised lymphatic organ located beneath the left diaphragm and the lower ribs. It is anchored by four ligaments, of which the splenocolic ligament, connecting the transverse colon to the splenic capsule, is the one most frequently injured during colonoscopy (3, 4). The exact mechanism of injury is unclear, but it is thought to result from increased traction on the splenocolic ligament, leading to capsular damage and splenic laceration. Adhesions between the spleen and colon, as well as other conditions that reduce mobility between these two structures, are considered contributing factors (3, 5).
Symptoms of splenic injury are often nonspecific. They typically present as gradually worsening abdominal pain, either diffuse or localised in the upper left quadrant. Some patients report pain radiating to the left shoulder (Kehr's sign), interpreted as a result of irritation of the left hemidiaphragm. Patients can rapidly develop signs of haemorrhagic shock, such as tachycardia, rapid breathing and hypotension (4).
In most cases of splenic injury secondary to colonoscopy, symptoms develop within 24 hours of the procedure, but they can appear with up to a ten-day delay (6).
The potentially serious course of splenic injury makes early diagnosis important. The recommended imaging modality for detecting splenic injury is CT with intravenous contrast (4, 5). The scan is primarily performed in the portal venous phase, but a supplementary arterial phase can be valuable for identifying ongoing bleeding.
The annual number of colonoscopies is gradually increasing in Norway (7), likely due to the introduction of the bowel cancer screening programme in 2022, as well as the steadily growing older population. In light of this, increased awareness of colonoscopy-related complications and their management is essential.
The patient has consented to publication of the article.
The article has been peer-reviewed.
- 1.
Dixe de Oliveira Santo I, Sailer A, Solomon N et al. Grading Abdominal Trauma: Changes in and Implications of the Revised 2018 AAST-OIS for the Spleen, Liver, and Kidney. Radiographics 2023; 43. doi: 10.1148/rg.230040. [PubMed][CrossRef]
- 2.
Wherry DC, Zehner H. Colonoscopy-fiberoptic endoscopic approach to the colon and polypectomy. Med Ann Dist Columbia 1974; 43: 189–92. [PubMed]
- 3.
Mallepally N, Bollipo S. Splenic Injury in Colonoscopy. Prevention, Management & Malpractice Issues. Gastroenterology & Endoscopy News 2023.
- 4.
Prowda JC, Trevisan SG, Lev-Toaff AS. Splenic injury after colonoscopy: conservative management using CT. AJR Am J Roentgenol 2005; 185: 708–10. [PubMed][CrossRef]
- 5.
Sarhan M, Ramcharan A, Ponnapalli S. Splenic injury after elective colonoscopy. JSLS 2009; 13: 616–9. [PubMed]
- 6.
Shankar S, Rowe S. Splenic injury after colonoscopy: case report and review of literature. Ochsner J 2011; 11: 276–81. [PubMed]
- 7.
Huppertz-Hauss G, Tarangen M. Gastronet. Årsrapport for 2023. https://www.sthf.no/49dafe/siteassets/underomrade-gastronet/arsrapporter/2023-arsrapport-gastronet.pdf Accessed 24.2.2025